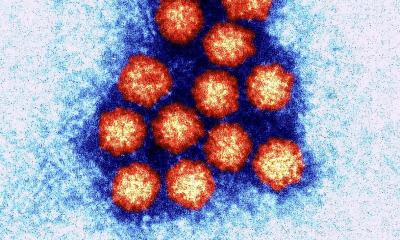
News • Research on medical communication
How healthcare can address vaccine hesitancy
Doubts about vaccination continue to be a significant challenge for global public health. The World Health Organisation (WHO) has listed vaccine hesitancy as one of the top ten threats to global health.

Image source: Maastricht University
But what exactly is vaccine hesitancy and how does it impact our society? How can we address it, particularly in healthcare? PhD candidate Veja Widdershoven conducted research into these questions and proposed ways to approach vaccine hesitancy.
Vaccine hesitancy refers to resistance or reluctance towards vaccination, often due to fear, mistrust, or misinformation. This can lead to preventable disease outbreaks and delays in herd immunity. Widdershoven’s research examines the complex factors that influence vaccine hesitancy and acceptance in the Netherlands. Her findings highlight the need for tailored strategies in vaccination communication.
Doubts around vaccination often arise from a lack of urgency, logistical or emotional barriers, and misinformation. “Misinformation has a very large impact,” Widdershoven notes. “It creates a sort of bubble. The only way to combat this is to keep repeating the correct information. You can’t stop people from posting online, so we need to put our own correct information in the spotlight, again and again and again.”

Widdershoven believes that building trust should be at the core of public health efforts. “It’s not about persuading those who are firmly against vaccines but rather about supporting the larger group of people who are unsure or seeking answers,” she explains. Society will benefit more from providing accurate information to this group than from trying to convince those who remain strongly opposed to vaccination.
We don’t want to push anybody to vaccinate. We want to make sure that people have the right information to make the right decision for themselves
Veja Widdershoven
Widdershoven also advocates for regional policy changes rather than national mandates. Vaccination strategies that work in cities like Amsterdam, for example, may not be as effective in regions like South Limburg. This is due to differences in population density, healthcare accessibility, and local infrastructure. In Amsterdam, for instance, a vaccination centre located in a central building is more easily accessible to many people. In South Limburg, on the other hand, reach may be limited due to the spread of smaller villages and the greater distances between populations. Additionally, urban areas like Amsterdam could benefit more from digital appointments, while rural areas like South Limburg, face-to-face communication and mobile vaccination units could be more effective.
Not only the location, but the timing of vaccination also plays an important role. Strategies used during the Covid-19 pandemic differ greatly from strategies for pregnant persons needing vaccination against diseases like whooping cough. During the Covid-19 pandemic, mass communication campaigns, targeted outreach to high-risk groups, and information distribution through multiple channels were employed. In a global pandemic, rapid and targeted communication is crucial to prevent panic and distrust. For whooping cough, the focus is instead on delivering targeted information to one specific group of people, namely pregnant individuals. In this situation, there is much more time for education.
To reduce doubts about vaccination and thereby increase vaccination rates, Widdershoven proposes several strategies that healthcare providers can apply:
- Motivational interviewing: This method uses open, non-judgemental conversations to help those unsure about vaccination understand their concerns and make a decision. It strengthens trust and helps the person make informed choices about their health.
- Improving accessibility: Access to vaccines can be increased by offering flexible appointment times, using multilingual and visual materials, and enhancing communication for people with varying levels of health literacy.
Widdershoven’s findings offer an optimistic perspective. It is not that most people are fundamentally opposed to vaccination, they need support in making informed decision about whether or not to get vaccinated. This is the exact approach Widdershoven proposes in her research: “We don’t want to push anybody to vaccinate. We want to make sure that people have the right information to make the right decision for themselves.”
Widdershoven’s research provides a framework for healthcare providers to address vaccine hesitancy. This framework allows for an approach that respects individual choice while promoting the well-being of both the community and the individual.
Source: Maastricht University; text: Rianthe Angela
20.01.2025