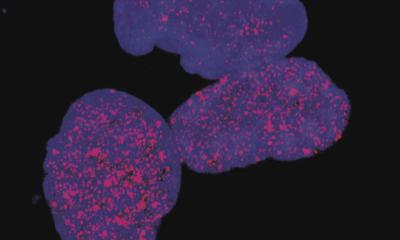
Credit: Caroline Contat (EPFL)
News • Neutrophil
Glucose is the key for lung cancer resistance
Lung tumors are home to immune cells that affect their growth and resistance to treatment. Looking at neutrophils, scientists led by EPFL have discovered that the key might lie in the cells’ ability to metabolize glucose, opening an entirely new target for improving radiotherapy.
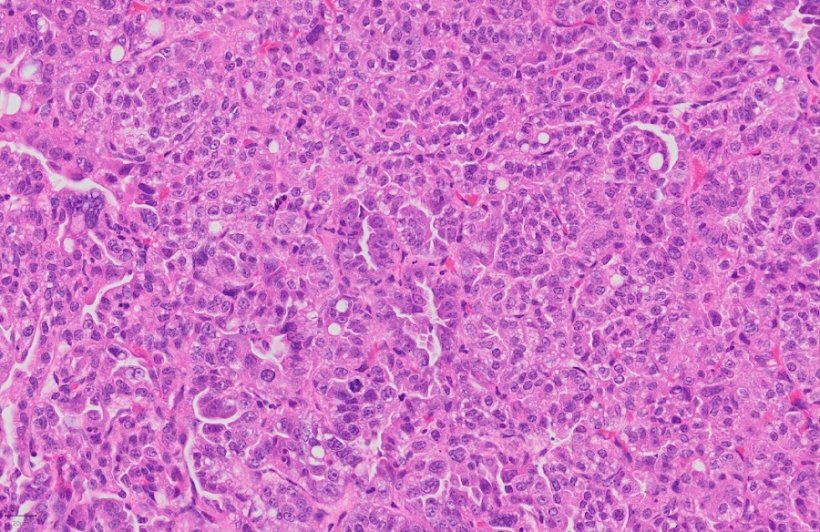
Cancers are not only made of tumor cells. In fact, as they grow, they develop an entire cellular ecosystem within and around them. This "tumor microenvironment" is made up of multiple cell types, including cells of the immune system, like T lymphocytes and neutrophils.
The tumor microenvironment has predictably drawn a lot of interest from cancer researchers, who are constantly searching for potential therapeutic targets. When it comes to the immune cells, most research focuses on T lymphocytes, which have become primary targets of cancer immunotherapy—a cancer therapy that turns the patient's own immune system against the tumor.
But there is another type of immune cell in the tumor microenvironment whose importance in cancer development has been overlooked: neutrophils, which form part of the body's immediate or "innate" immune response to microbes. The question, currently debated among scientists, is whether neutrophils help or inhibit the tumor's growth.
Now, a team of researchers led by Etienne Meylan at EPFL's School of Life Sciences has discovered that the metabolism of neutrophils determines their tumor-supportive behavior in lung cancer development. The study is published in Cancer Research, a journal of the American Association for Cancer Research.
Credit: Liloon (Julie de Meyer)
What intrigued the scientists was that cell metabolism in cancer becomes deregulated. Being neutrophil specialists, they considered the possibility that when these cells reside within the tumor microenvironment, their metabolism may also change, and that could affect how they contribute to the cancer's growth.
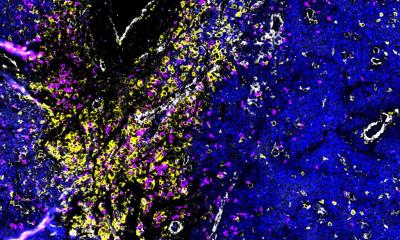
Focusing on glucose metabolism in a genetically engineered mouse model of lung adenocarcinoma, the scientists isolated tumor-associated neutrophils (TANs) and compared them to neutrophils from healthy lungs.
What they found was surprising: the TANs take-up and metabolize glucose much more efficiently than neutrophils from healthy lungs. The researchers also found that TANs express a higher amount of a protein called Glut1, which sits on the cell's surface and enables increased glucose uptake and use.
To understand the importance of Glut1 in neutrophils during lung tumor development in vivo, we used a sophisticated system to remove Glut1 specifically from neutrophils," says Pierre-Benoit Ancey, the study's first author. "Using this approach, we identified that Glut1 is essential to prolong neutrophil lifespan in tumors; in the absence of Glut1, we found younger TANs in the microenvironment."
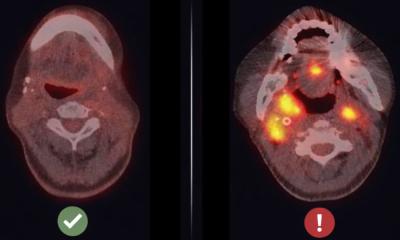
Using X-ray microtomography to monitor adenocarcinomas, the researchers found that removing Glut1 from TANs led to lower tumor growth rate but also increased the efficacy of radiotherapy, a common treatment for lung cancer. In other words, the ability of TANs to metabolize glucose efficiently seems to bestow the tumor with the ability to resist treatment—at least in lung cancer.
The scientists think that, because Glut1 loss diminishes the lifespan of TANs, their "age" determines whether they play a pro- or anti-tumor role. "Usually, we don't know how to target neutrophils, because they are so important in innate immunity," says Etienne Meylan. "Our study shows that their altered metabolism in cancer could be a new Achilles heel to consider in future treatment strategies. Undoubtedly, we are only beginning to learn about these fascinating cells in cancer."
Source: École Polytechnique Fédérale de Lausanne
23.03.2021