News • Alteration of immune response
Multiple myeloma: dangerous diversity
A research team from the Heidelberg Medical Faculty, the German Cancer Research Center (DKFZ), the Berlin Institute of Health at Charité (BIH) and the Max Delbrück Center has discovered new details about the spread of the incurable bone marrow cancer multiple myeloma in the body:
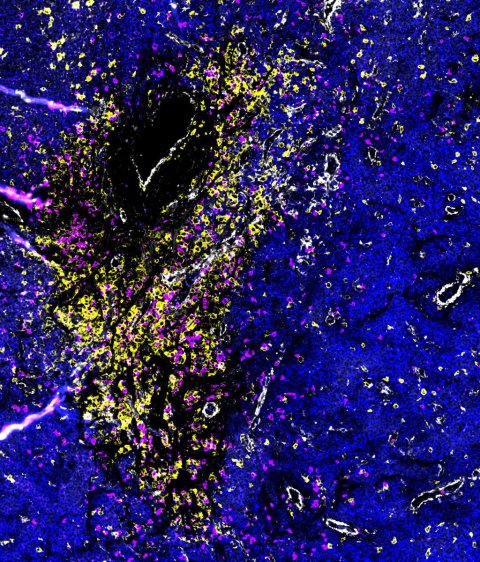
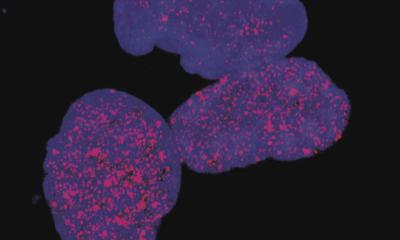
Image source: Dr. Johanna Wagner, DKFZ and NCT Heidelberg, acquired using spatial multi-omics methods.
When the cancer cells break out of the bone and multiply outside the bone marrow, a wide variety of tumor cells arise, accompanied by a significantly altered immune response. The findings, published online in the journal “Science Immunology,” could be crucial for the further development of diagnostics and therapy.
Multiple myeloma, an incurable type of bone marrow cancer, often develops unnoticed in the bone marrow over decades. In advanced stages, lesions form that can destroy the bone and spread to other parts of the body. An interdisciplinary team from the Myeloma Center at Heidelberg University Hospital (UKHD), Heidelberg University, DKFZ, BIH and the Max Delbrück Center together with other national and international partners have been investigating what happens in these lesions when the myeloma cells first break out of the bone. The researchers discovered that the tumor cells develop a dramatic diversity when leaving the bone marrow, which also affects the immune cells in the cancer foci. The new findings could contribute to more precise diagnostics and therapy.
When the tumor cells leave the bone marrow and also the bone, they find themselves in a completely different environment with different environmental conditions. “This apparently acts as an evolutionary boost for the tumor cells. The diversity that arises in the process could help the cells to adapt to survival outside the bone and enable them to spread to other parts of the body,” says Dr. Niels Weinhold, head of Translational Myeloma Research at the UKHD's Department of Hematology, Oncology and Rheumatology and the Heidelberg Medical Faculty.
This interaction between the immune system and cancer could both promote and hinder the fight against it. We are currently investigating which factors play a positive or negative role in this process
Simon Haas
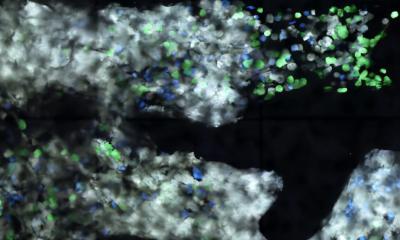
Using innovative technology, the team also examined for the first time how the immune system reacts to this “outbreak” of cancer cells from the bone. They discovered significant changes in the type and number of immune cells in the area of the cancerous lesions. For example, certain immune cells, known as T cells, had very different receptors and surface molecules in the foci outside the bone – a possible adaptation to the newly emerged heterogeneity of the tumor cells. “There seems to be a kind of co-evolution between tumor and immune cells, in which both sides react to changes in the other,” says Professor Dr. Simon Haas, a precision medicine specialist at the BIH, the Max Delbrück Center and the Precision Healthcare University Research Institute (PHURI) of the Queen Mary University of London. “This interaction between the immune system and cancer could both promote and hinder the fight against it. We are currently investigating which factors play a positive or negative role in this process.”
The tissue material examined came from various myeloma lesions in newly diagnosed patients, either from imaging-guided biopsies or during surgery on fragile or already fractured bones. Modern single-cell analyses and spatial multi-omics techniques were used. These methods allow the simultaneous investigation of various properties of thousands of single cells in the tissue, taking into account its exact position in the tissue.
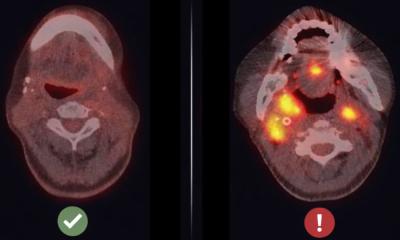
The results could influence the diagnosis and therapy of myeloma in the future: Currently, samples for diagnosis are usually taken from the iliac crest of patients. However, since the study has now shown that cancer and immune cells in bone openings differ significantly from those in the iliac crest, these sites may be better suited for sample collection, allow a more precise assessment of the disease and possible adjustment of therapy.
First authors of the article are Dr. Alexandra Poos, Dr. Raphael Lutz and Dr. Lukas John, researchers at the Heidelberg Medical Faculty of Heidelberg University and the DKFZ, as well as Dr. Llorenç Solé Boldo, scientist at the Max Delbrück Center, BIH and PHURI.
Source: Heidelberg University Hospital
12.02.2025