Gene therapy restores sense of smell in mice
A team of scientists from Johns Hopkins and other institutions report that restoring tiny, hair-like structures to defective cells in the olfactory system of mice is enough to restore a lost sense of smell.
The results of the experiments were published online this week in Nature Medicine, and are believed to represent the first successful application of gene therapy to restore this function in live mammals.
An expert in olfaction, Randall Reed, Ph.D., professor of molecular biology and genetics and co-director of the Center for Sensory Biology at the Johns Hopkins Institute for Basic Biomedical Sciences, cautions that researchers are still years away from applying the same therapy in people, and that if and when it comes, it will likely be most effective for those who suffer from anosmia (lack of smell) due to inherited genetic disorders. “But our work has already contributed to a better understanding of the cellular factors involved in anosmia, and that will give us insights into other neurological disorders, as well,” he says.
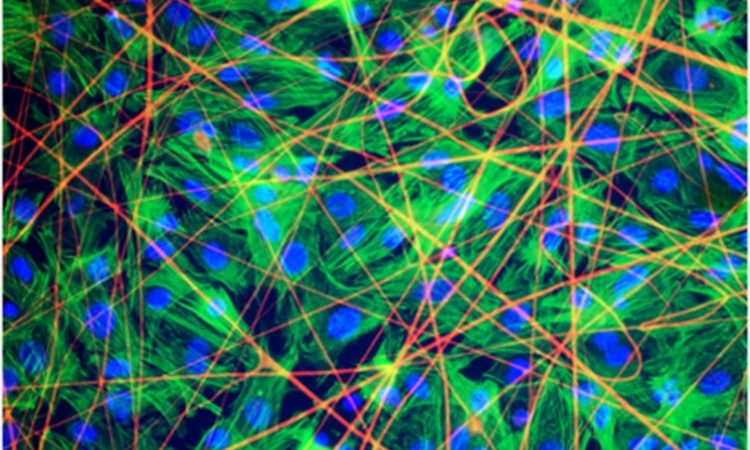
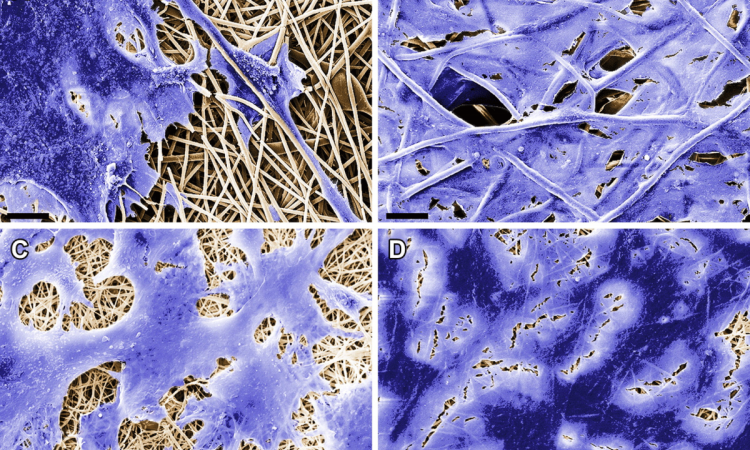
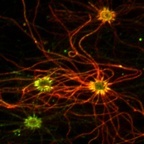
The mice used in the current study carried a genetic mutation that destroyed the production of a protein critical for the functioning of cilia in the cells responsible for smell, called olfactory sensory neurons. These specialized cells each display several of the protruding, hair-like structures that contain receptors for odorants. Without functional cilia, the cells become a broken link in the chain of events necessary for proper odor detection in the environment, the researchers explained.
Beginning with a common cold virus, which readily infects the cells of the nasal cavity, researchers replaced some of the viral genes with a corrected version of the defective cilia gene. They then infected smelling-impaired mice with the altered virus, delivering the corrected gene to the olfactory neural cells that needed it.
At the cellular level, scientists saw a restoration of proper chemical signaling between nerve cells after the treated mice were stimulated with various odorants. Perhaps even more indicative of their success, Reed says, was the 60 percent increase in body weight that the mice experienced once they could smell their meals, leading to increased appetite. Many people with anosmia lose weight because aromas play a significant part in creating appetite and food enjoyment.
Researchers are optimistic about the broader implications of this work, Reed notes, because cilia are not only important to olfactory cells, but also to cells all over the body, from the kidney to the eye. The fact that they were able to treat live mice with a therapy that restored cilia function in one sensory system suggests that similar techniques could be used to treat cilia disorders elsewhere.
“We also hope this stimulates the olfactory research community to look at anosmia caused by other factors, such as head trauma and degenerative diseases,” says senior author Jeffrey Martens, Ph.D., an associate professor of pharmacology at the University of Michigan. “We know a lot about how this system works – now have to look at how to fix it when it malfunctions.”
In addition to Randall Reed from Johns Hopkins, the paper’s authors include Jeffrey Martens, Jeremy McIntyre, Ariell Joiner, Corey Williams, Paul Jenkins, Dyke McEwen, Lian Zhang and John Escobado from the Martens Lab at the University of Michigan; Erica Davis, I-Chun Tsai and Nicholas Katsanis from Duke University; Aniko Sabo, Donna Muzny and Richard Gibbs from the Baylor College of Medicine; Eric Green and James Mullikin from the National Institutes of Health Intramural Sequencing Center; Bradley Yoder from the University of Alabama-Birmingham; Sophie Thomas and Tania Attié-Bitach from L’Université Paris Descartes; Katarzyna Szymanska and Colin A. Johnson from St. James’s University Hospital in Leeds, UK; and Philip Beales from University College London, UK.
The study was funded by the National Institutes of Health: National Institute on Deafness and Other Communication Disorders (#R01DC009606, F32DC011990, R01DC004553, R01DC008295), National Institute of Diabetes and Digestive and Kidney Diseases (#R01DK75996, R01DK072301, R01DK075972, DK074083), National Institute of Child Health and Human Development (#R01HD042601), and National Eye Institute (#R01EY021872). Additional funding sources included L’Agence Nationale de la Recherche and the European Community’s Seventh Framework Programme.
10.09.2012