News • Study on antiviral therapy efficacy
Covid-19 treatment of immunocompromised patients: better late than never
Starting antiviral treatment as late as 14 days after infection with Sars-CoV-2 may still be beneficial in hosts with compromised immune systems, who are at greatest risk of developing severe Covid-19, according to researchers in the Center for Translational Antiviral Research at Georgia State University’s Institute for Biomedical Sciences.

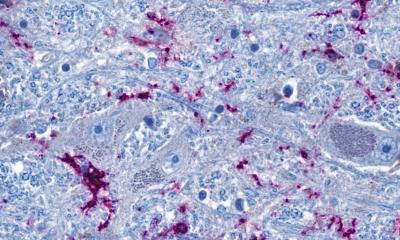
Image credit: Georgia State University
While best to begin treatment earlier, in immunocompromised hosts, drugs like paxlovid and molnupiravir appear to inhibit replication of the virus even if initiated up to 14 days after infection.
The study, published in the Journal of Virology, offers new information about late-onset treatment introduced 14 days after infection with Sars-CoV-2, the virus that causes Covid-19. The findings demonstrate that antiviral therapeutics could have valuable clinical use in late-onset management of persistent Sars-CoV-2 infection in immunocompromised patients, in addition to reducing the risk of progression to severe disease.
The researchers sought to offer specific Sars-CoV-2 treatment plans to the immunocompromised and tested late-onset therapeutic options with standard-of-care paxlovid and molnupiravir and experimental therapeutic 4’-Fluorouridine (4’-FlU) in a T-cell depleted immunocompromised mouse model of Sars-CoV-2.
The Centers for Disease Control and Prevention (CDC) recommends that individuals with impaired immune functions use antivirals and immunomodulatory drugs at the doses and durations similar to the general patient population, but this new study indicates benefits of late treatments to mitigate persistent viral replication, the authors explained.
“Paxlovid, molnupiravir and pre-clinical candidate 4’-FlU significantly lowered virus loads in turbinates (bony structures in the nose that regulate airflow and warm and humidify air that is inhaled) when treatment was initiated 14 days after the infection for seven days,” said Dr. Carolin M. Lieber, first author of the paper and a postdoctoral fellow in the Center for Translational Antiviral Research at Georgia State.

Image credit: Georgia State University
“We demonstrated that late-onset antiviral treatment can provide major therapeutic benefit to an immunocompromised host infected with Sars-CoV-2,” said Dr. Richard K. Plemper, senior author of the study, Regents’ Professor and Director of the Center for Translational Antiviral Research at Georgia State. “This study highlights that appropriately powered clinical trials are urgently needed to best serve the specific needs of a patient population at high risk to develop severe Covid-19.”
In the study, immunocompromised mice experienced low-level viral replication for 35 days after the infection with Sars-CoV-2. When started on antivirals 14 days after infection, however, the duration of virus replication was significantly shortened, which could have implications for clinical usage of antiviral drugs in immunocompromised patients.
Additional authors of the study include Hae-Ji Kang, Vu Ngo and Andrew Gewirtz of the Institute for Biomedical Sciences at Georgia State; Elizabeth Sobolik and Alexander Greninger of the University of Washington Medical Center; Zachary Sticher, Alexander Kolykhalov and Michael Natchus from the Emory Institute for Drug Development; and Mehul Suthar from the Emory University School of Medicine.
Source: Georgia State University
06.09.2024