
Source: Pixabay/ulleo
News • In 2020
COVID-19 restrictions linked to 750,000 fewer dengue cases
New study shows COVID-19 measures such as school closures and ‘high-traffic and mixing’ areas had the strongest association, providing clues for new intervention approaches.
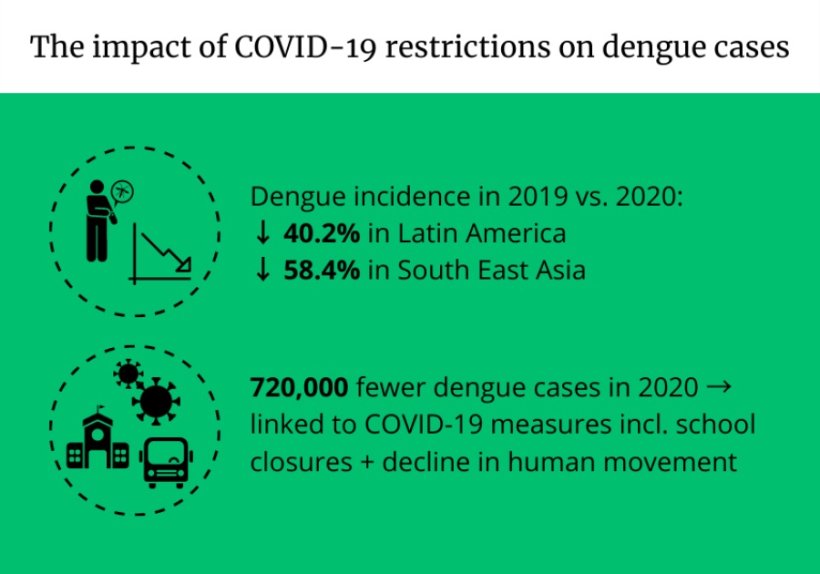
Nearly three quarters of a million fewer global cases of dengue occurred in 2020, which could be linked to COVID-19 disruptions limiting human mobility and contact, according to a new study published in Lancet Infectious Diseases.
Researchers from the London School of Hygiene & Tropical Medicine (LSHTM), Beijing Normal University and other international partners, funded by the Medical Research Council, analysed the monthly dengue cases from the World Health Organization (WHO) Weekly reports between 2014 to 2020 from 23 countries – 16 in Latin America and seven in South East Asia, the main regions where dengue is endemic, as well as climate data on air temperature, relative humidity and precipitation.
They found a strong association between school closures and declines in non-residential trips, such as shopping or using public transport, due to COVID-19 and reduced risk of dengue transmission. This indicates that places such as schools and commonly visited public areas could be dengue transmission hot spots and play a key role in spreading the disease.
Further research is needed into how human movement behaviours (the places people visit, how long they spend there and with whom) impact dengue transmission risk. This could help decision makers decide if measures like contact tracing, testing or quarantine could help control the spread of the disease.
Source: London School of Hygiene and Tropical Medicine
Dr Oliver Brady, Associate Professor and MRC Fellow at LSHTM and study senior author, said: “Currently dengue control efforts are focused on or around the households of people who get sick. We now know that, in some countries, we should also be focusing measures on the locations they recently visited to reduce dengue transmission. For all the harm it has caused, this pandemic has given us an opportunity to inform new interventions and targeting strategies to prevent dengue.”
Dengue is a viral infection transmitted by the Aedes species of mosquitoes, which causes flu-like symptoms. It is found in tropical and sub-tropical climates worldwide, and is most common in urban areas.
It is one of the only infectious diseases to show a sustained increase in cases each year, and the WHO now estimates that around half the world’s population is at risk of contracting dengue.
Transmission is closely linked to the weather, surrounding environment and human mobility. It is also closely associated with the climate, with hot and humid tropical climates ideal for transmission. Dengue season in many countries occurs around June to September, when peaks in cases can cause overcrowding in hospitals – much like with COVID-19.
Dengue is only spread from mosquito to human and vice versa, and is not transmitted from humans to other humans. However, changes in people’s movements and behaviour may have an effect on transmission, for example through reduced exposure to mosquitoes or fewer opportunities for infected people to go out and about and pass on the virus to uninfected mosquitoes present there. COVID-19 and the restrictions on human movement that were imposed during the pandemic therefore provide a unique opportunity to explore how human movement and behaviour contribute to dengue transmission.
Dengue case numbers suddenly began to decline in April 2020 in many countries, following the introduction of public health and social measures targeting the spread of COVID-19 and the resulting change in human movement and shift to more time spent in residential places. In 2020, dengue cases decreased by 40.2% in Latin America and 58.4% in South East Asia, with just over two million cases recorded in the Americas and South East Asia in 2020.
However, unravelling the impacts of COVID-19 disruption is complex as 2019 saw the largest global dengue outbreak in history, with more than 5.2 million cases recorded in the Americas and South East Asia region. This led to high levels of immunity which would also be expected to reduce dengue cases in 2020.
Dr Brady added: “Before this study, we didn’t know whether COVID-19 disruption could increase or decrease the global burden of dengue. While we could assume reduction in human movement would reduce the virus transmission, it would also disrupt the mosquito control measures already in place. This disruption may result in long-term impacts on dengue cases which might not be evident until the next epidemic.”
The research team looked at two different measures of COVID-19 related disruption – public health and social measures, such as school and public transport closure, stay-at-home requirements, gathering restrictions; and human movement behaviour through time spent at residential and public locations. They also accounted for the different strengths of restrictions in lockdowns in different countries around the world.
By combining all this data and analysing trends, they were able to show that reduced time spent in public areas was closely associated with reduced dengue risk.
Nine out of 11 countries in Central America, the Caribbean and the Philippines saw a complete suppression of their 2020 dengue season, with other countries experiencing a much reduced season. In countries where the COVID-19 restriction measures began at the peak of dengue season, there was a sharper than expected decline in cases, despite above average incidence being recorded earlier in the year.
This decrease in cases could also be attributed to reduced rates in people seeking treatment, a higher potential for misdiagnosis and reduced availability for laboratory testing for dengue could result in misdiagnosis. However, some countries such as Sri Lanka predicted this could be a problem at the start of the pandemic, so undertook outreach work to encourage people to get diagnosed and seek treatment. Despite this, there was no change in rates of severe cases and deaths reported, suggesting the reduction in treatment seeking was not the cause for the reduction in cases.
A better understanding of how treatment-seeking behaviours change during an epidemic is needed, as access to care and rapid diagnostics change in order to fully assess and interpret the change in case numbers. The team emphasises the need for longer term, more routine measurement of the prevalence of dengue within each population.
Although overall cases declined in 2020, Peru and Singapore reported worse than average dengue incidence in 2020. This could have occurred due to the unpredictable natural year-to-year variation in dengue incidence that occurs due to, for example, the emergence of different dengue virus variants, or could hint at the greater role being bitten by mosquitoes at home plays in spreading dengue in these countries.
As the climate recorded in 2020 was similar to the average climate of the last six years, the researchers did not find an association between climate and the reduction in dengue risk during 2020.
The researchers note that it remains to be seen how many of the estimated 0.72 million cases were truly averted, or just delayed until later years as human movement returns to pre-COVID levels and say it’s key to continue monitoring dengue trends in 2022 and beyond.
The researchers acknowledge the limitations of this study, including lack of data on the different types of dengue, which can drive outbreaks, and the potential changes in dengue reporting resulting from COVID-19 disruptions.
Source: London School of Hygiene and Tropical Medicine
07.03.2022





