Interview • Social care during the coronavirus pandemic
COVID-19: Don't forget the most vulnerable people
The COVID-19 pandemic has brought more strain on healthcare systems but it has also highlighted the necessity to integrate social care to healthcare to protect the most vulnerable populations in ageing societies, an eminent healthcare consultant told us in an exclusive interview.
Interview: Mélisande Rouger
This profound crisis is an opportunity for change, but the world needs good leaders to ride the wave, according to Rafael Bengoa, who helped shape health care systems in Spain and beyond from within the World Health Organization.
HiE: What are the strengths of the Spanish public healthcare system?

Bengoa: Spain has a good coverage in terms of equity and access, as every other European country. Our healthcare system is a public, compulsory NHS-type of Beveridge system. About 20% of the population has a combined public and private healthcare plan.
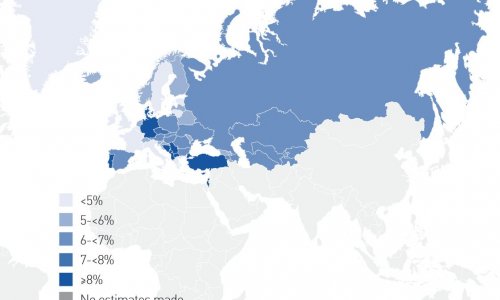
It’s difficult to benchmark countries as to who has the best system. Ours is good, but not when it comes to chronic patients. Actually, there isn’t a single country in the world with a good, efficient system that provides continuity of care to patients with diabetes, hypertension, cardiac and other chronic diseases for decades. Chronicity should be better managed all across the world. It’s a global problem. Vulnerable people have to be more on the radar and not only during epidemics! That’s especially true for Spain, but also Italy and Greece, where many people are over 100 years old. But young people may also have diabetes, and these patients will have to be monitored during their whole life. They need a supportive system and it’s not the one we currently have.
How would you describe the Spanish response to the pandemic?
The response in Europe and Asia has been correct and based on scientific thinking both epidemiologically and clinically. The relationship between science and politics is not a given as we can see in the U.S., Brazil and Mexico. Many purely political leaders have been assuming a scientific role. That is not the way forward in such a crisis. In general, the response here has been late, like everywhere else. We lost a good part of the month of February. The same can be said about our level of pandemic preparedness. It was insufficient, as everywhere else.
Recommended article

Article • Coronavirus chronology
COVID-19 in the U.S.: Government inaction gave virus a head start
The sense of fear is palpable in the images and videos of hospital intensive care units (ICUs) and emergency departments that are broadcast on television and posted on social media. Fear and heartbreak can be heard in the voices of physicians and nurses who describe what they are experiencing.
Why have we been late compared to other European countries?
I think that countries like Germany were not as surprised as Spain or Italy in terms of volume and speed of community transmission. The most likely assumption is that Germany and Nordic countries don’t face similar family transmission – 70% of Swedes and 50% of Germans live alone. In Italy and Spain, 70% of the people live in close contact with their family. That may have made a big difference in the way we have been exposed.
We need to ensure that public health is strengthened quickly, in order to also control infectiousness in the community
Rafael Bengoa
After the SARS outbreak in 2002-2004, most European countries ignored the warnings issued by the WHO that another, bigger epidemic was coming. Nobody prepared for this one. It’s not surprising that we’ve been more unprepared than the Asians, who have more outbreaks and are ready for these. Asian countries have more potential for such outbreaks because of their relationship with animals. They have a hard time changing that, so they know they’re going to have more problems with viruses jumping from animals to humans.
During this COVID epidemic, Spain has been very focused on the more dramatic side of things, i.e. the acute phases of the disease, the ICUs. That has deviated our attention. We should have focused simultaneously on massive testing in the community. The healthcare system has been resilient and strong, but we need to ensure that public health is strengthened quickly, in order to also control infectiousness in the community.
Image source: Unsplash/Ryoji Iwata
Was the Spanish healthcare system properly equipped to respond to this outbreak?
The Spanish HC system is a well-oiled machine and it’s affordable to everyone. It has resources, as Spain has invested efforts and money for the past 30 years. So we can assume that we had the proper system to respond. But we certainly didn’t have the necessary equipment. Again, neither did Canada, the U.S., Australia and so many other countries. One of the lessons we’re all learning is: when an epidemic hits again, we must make sure we have “surge” capacity, i.e. that we can create the equipment nationally and don’t need to go into any type of radical international market competition, as has happened on this occasion. We need to make sure that we have six or seven infrastructures that can make all these equipment relatively quickly. A facemask that is made today won’t be usable in ten years. So you have to have some reserve, but also the capacity to make the equipment rapidly.
What other lessons have we learned from this experience? Is using war-like terminology useful or does it just create more panic?
We cannot have elderly patients in nursing homes and not know what is going on with them
Rafael Bengoa
War-like semantic is probably useful to have people slightly concerned. In a way we are in a sort of war, so I’m not surprised people use terms like health war, escalation, de-escalation, etc.
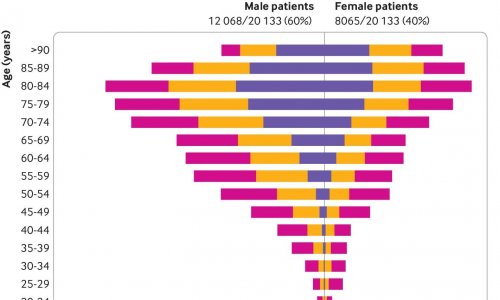
More than the semantics, I think that a huge flaw in this crisis was the structural exposure of the weak relationship between health and social care. Two thirds of deaths in Spain have been people aged 70 years and above. The reason is not only because that was biologically the most vulnerable group, but also because of the organisational arrangement we have between health and social care. It’s important that we start connecting long-term social care with healthcare. They need to be better protected. We cannot have elderly patients in nursing homes and not know what is going on with them.
In New Zealand, the District Health Board for Canterbury, the south island’s most populous region, has launched an initiative to provide care that crosses the boundaries between primary, community, hospital and social care about five years ago. That is a model we need to be looking at. This epidemic is an opportunity to get this right.
Recommended article

Article • Meeting of the generations
We need a Senior Laboratory
It’s undeniable: the bulk of our population is growing older. Yet, this demographic change has not altered laboratory medicine: the reference values for many analyses are still based on data of a younger cohort. Inevitably this could lead to serious errors in the interpretation of older patients’ test results.
Was it necessary to have an outbreak this size for politics to become aware of these needs?
All big crises, including the 1929 economic crisis, which impoverished the whole world, also had some good consequences. That’s when successive U.S. and European presidents were able to introduce massive welfare state types of arrangements, for example the creation of the National Health Service in the UK and the Sécurité Sociale in France after WW2. The important thing is to have good leaders to manage these opportunities. If we don’t have good leaders, we won’t have these changes.
Do we have good leaders now?
Citizens have been asked to be actors in this crisis and not only passive recipients of services. Citizens now have the right to request real leadership form their politicians. We can’t leave it only up to them. Leaders will need independent and impartial depoliticized reports of this crisis: what happened, why that happened and how to ensure it doesn’t happen again at this level of health and economic impact. Simultaneously to this challenge, we have to prepare our system for an ageing society in a way that is more effective and economically sustainable.
We’ve had more than ten years of significant cuts in the health care budget in Spain
We had a hard time with the financial crisis in 2009. Spain was hit much harder than Germany and France. Portugal, Ireland and other countries had to be intervened in financial terms. We avoided it just barely. That’s when I was appointed health minister for the Basque Country. It was a very tough time. Both national and regional ministers had to take tough decisions. Some of the cuts we made included freezing some salaries nationally. It was an opportunity to make our system more efficient and many reforms were launched in 2010 in digital health, integrated care and management of chronic conditions.
Did decentralization of healthcare services help to manage the epidemic?
Decentralized Spain has improved health outcomes across the country; such an organization has created a stronger management capacity.
In France, President Macron announced a few months ago that he wanted to decentralize HC to the regions (i.e. the Decentralization Act on safety, ecological transition and education and health). During an outbreak, when you don’t know how much community transmission is going on in the country, it’s better to have less population movement.
In Spain, during the steepest rise of the epidemic, most patients were treated in their community. The decision was to strengthen and build hospitals locally and not to move patients. This was a legitimate decision in the sense it worked correctly.
What will be the outcome of the epidemic in less developed countries?
Hopefully this pandemic will make us better understand the more constructive interrelationships that are necessary in a globalized world
Rafael Bengoa
If we have a hard time in a fairly structured country with a fairly structured healthcare system, imagine what this is going to be where they don’t have either. I believe it is going to be very dramatic unless we discover a treatment and vaccine fairly quickly.
We have to stop only looking at ourselves in the developed world. The WHO needs to look at these countries. Most of them won’t have the economic leverage we have. A lot of people are going to die unnecessarily. Hopefully this pandemic will make us better understand the more constructive interrelationships that are necessary in a globalized world.
Will the legacy of the Affordable Health Care Act (ACA) help limit the damage in the U.S.?
It is extremely surprising that the U.S. do not have universal healthcare considering the amount invested in healthcare in that country. A country without universal coverage is not where you want to be when a crisis like this hits. I suppose this pandemic will reopen the debate on healthcare in the U.S. and it will probably have a significant impact on the forthcoming elections.
The ACA has probably helped limit the damage, but even today, 15% of the population remains without any insurance and another 50 million Americans are not well covered. We all hope the Americans can find a quick solution that is based on their culture.
Profile:
Rafael Bengoa is a trained physician and health management consultant who is currently co-heading the Health and Strategy Health Institute (SI-Health) in Bilbao, Spain. He is a strong advocate for universal healthcare and his work has been largely recognized, with numerous appointments worldwide. Bengoa was Healthcare Minister for the Basque Country between 2009 and 2012 and is considered a founding father of Osakidetza, the Basque public healthcare system. For 14 years Bengoa worked for the World Health Organization, where he was responsible for Health Systems until 2006. He has directly advised many countries regarding their healthcare policies including Ireland, Northern Ireland, Spain and the United States.
30.04.2020