Experts argue
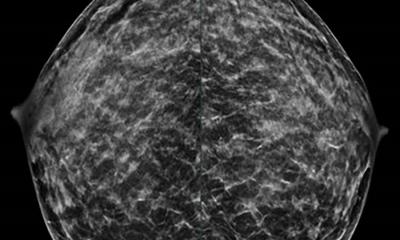
Cancer screening does not “save lives”
Harms of screening are certain, but benefits in overall mortality are not … “We must be honest about this uncertainty,” experts say. Cancer screening has never been shown to “save lives” as advocates claim, argue experts in The BMJ.
This assertion rests on reductions in disease specific mortality rather than overall mortality, say Vinay Prasad, Assistant Professor at Oregon Health and Science University and colleagues. They argue that overall mortality should be the benchmark against which screening is judged and call for higher standards of evidence for cancer screening. There are two chief reasons why cancer screening might reduce disease specific mortality without significantly reducing overall mortality, write the authors.
Firstly, studies may be underpowered to detect a small overall mortality benefit. Secondly, disease specific mortality reductions may be offset by deaths due to the downstream effects of screening. Such “off-target deaths” are particularly likely among screening tests associated with false positive results (abnormal results that turn out to be normal) and overdiagnosis of harmless cancers that may never have caused symptoms, they explain. For example, prostate cancer testing yields numerous false positive results, which contribute to over one million prostate biopsies a year - which, in turn, are linked to serious harms, including admission to hospital and death.
Men diagnosed with prostate cancer are also more likely to have a heart attack or commit suicide in the year after diagnosis or to die of complications of treatment for harmless cancers. Yet data has shown that the public has an inflated sense of the benefits and discounted sense of the harms of screening, they write.
For instance, in one study 68% of women thought that breast screening would lower their risk of getting breast cancer, 62% thought that screening at least halved the rate of breast cancer, and 75% thought that 10 years of screening would prevent 10 breast cancer deaths per 1000 women.
Yet they point out that the most recent Cochrane review of PSA screening trials “failed to show a reduction in disease specific death,” while their mammography review “did not show reduced breast cancer deaths when adequately randomised trials were analysed.”
Consideration of harms also becomes more important in the absence of clear overall mortality benefit, they add. Advocates of screening have emphasised its benefits, sometimes verging on fear mongering, note the authors. Others, including us, think that shared decision making should be the focus. “But as long as we are unsure of the mortality benefits of screening we cannot provide people with the information they need to make an informed choice. We must be honest about this uncertainty.”
To find out whether screening saves lives, they say investing in large trials that can determine overall mortality is “worth the expense compared with the continued cost of supporting widespread screening campaigns without knowing whether they truly benefit society.”
They acknowledge that political will, financial resources, and public perception “are common hurdles in building support for resource intensive scientific endeavours, and developing consensus on these matters will take time and effort.” And they call on healthcare providers “to be frank about the limitations of screening” and for higher standards of evidence “to enable rational, shared decision making between doctors and patients.”
In an accompanying editorial, Gerd Gigerenzer argues that "rather than pouring resources into 'megatrials' with a small chance of detecting a minimal overall mortality reduction, at the additional cost of harming large numbers of patients, we should invest in transparent information in the first place."
He explains that even if the uncertainty of screening on overall mortality is not removed, we can provide people with useful tools to help with informed decision making, adding that "it is time to change communication about cancer screening from dodgy persuasion into something straightforward."
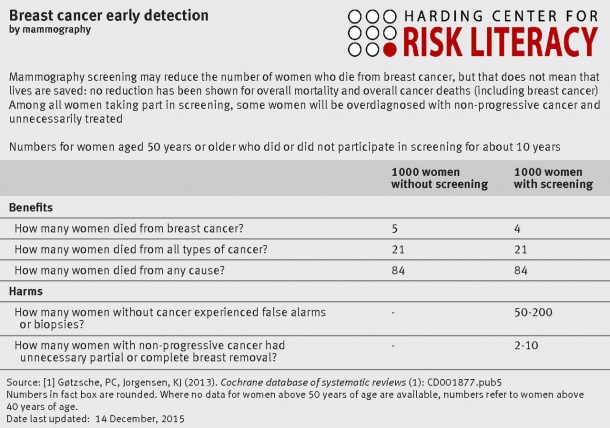
Useful tools such as fact boxes can illustrate harms associated with mammography screening, for example, by reporting all three measures of mortality (see article for an example). "The harms are specified numerically so that an informed decision about screening is possible. Every article and pamphlet should provide a fact box summary to facilitate informed decisions," he concludes.
Source: The BMJ
07.01.2016