Article • Lung cancer early diagnosis
Can we afford not to offer lung screening?
For lung cancer patients, life expectancy has hardly improved since 1970. A ten-year survival is 5%, making this the leading cause of death among all cancers. One reason is that, in most cases, the disease is diagnosed far too late.
Interview: Daniela Zimmermann
Image source: Shutterstock/Semnic
Previous evidence on the benefits of screening programmes to detect lung cancer early, was mainly based on data from the NLST study in the US (National Lung Screening Trial; N Engl J Med 2011), was considered insufficient. However, the publication of the Belgian-Dutch NELSON study (De Koning et. al, 2018) has just changed this. For the first time, lung cancer screening has moved within reach.
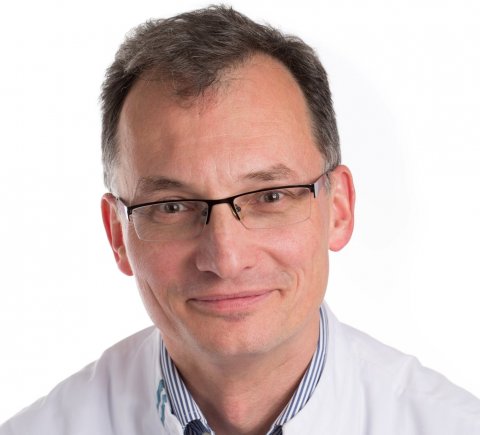
Professor Mathias Prokop, head of the Department of Radiology at Radboud University Hospital Nijmegen, is among leading advocates of low-dose CT screening for lung cancer for high risk patients. At this year’s congress, he explained aspects of the current debate in the context of the Holzknecht Lecture.
Considering present evaluation by the Federal Office for Radiation Protection (BfS) as to whether lung screening makes sense, what might be the main concerns?
Prokop: ‘First, the BfS obviously deals with radiation protection. As a result of new technology, radiation exposure during chest CTs now poses an almost negligible risk. In the NLST study, the dose per examination was between one and three mSv; in the NELSON study it was lower than one mSv. Some experts even say that they can screen with 0.2 - 0.1 mSv.
What the current evaluation procedure is really about is the assessment of the risk/benefit ratio, given false positives and over-diagnosis and treatment. There is a danger that patients who would never have died of lung cancer are exposed to the potential complications of an invasive medical procedure. If there is no need to intervene it should not be done.’
What is the false positive rate?
‘It depends what you define as positive. The NLST study classed all nodules larger than 4 mm as positive, which leads to an extremely high false positive rate of 96.4%. Those who carried out the study simply lacked empirical values because they were the first to analyse this. In all later trials, results were only classed as positive where further examinations were carried out because lung cancer was explicitly suspected.
Therefore, the false positive rate for the NELSON study was only 10-15%, depending on which screening round you looked at. There are now new suggestions as to how the false positive test results can be pushed below five percent. Then definitely this would be acceptable and considerably better than the results achieved in breast cancer screening.’
Recommended article

News • Early detection
Lung cancer: Why screening is especially beneficial for women
Is computed tomography suitable for detecting lung cancer at a very early stage and thus still well treatable? Scientists at the German Cancer Research Center have investigated this with the LUSI study started in 2007. The results of the study, which is funded by the Deutsche Forschungsgemeinschaft and the Dietmar Hopp Foundation, are now available.
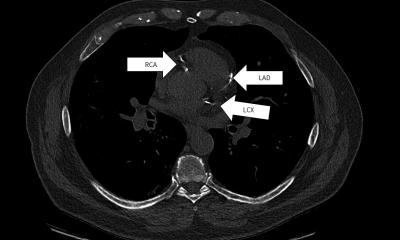
How does the radiologist detect lung cancer on a CT scan?
‘There are basically two methods that help us. There is morphology, where the size or the volume of a suspicious region plays the most important part. Then there are other morphological criteria that help with tumour determination, such as the shape or the localisation. A biopsy is only recommended for patients with large, high-risk pulmonary nodules. All other patients just receive follow-up examinations. This is where the second category comes into play: changes over time.
If the pulmonary nodule grows very fast, it is most likely to be a malignant tumour; if it grows slowly, it is likely to be either a benign tumour or a malignant tumour which the patient will live with until their death (from causes other than lung cancer). We must not forget that many patients who are recruited for lung screening are already multimorbid, because of their age and additionally they may, for instance, be at higher risk of a heart attack or a stroke.’
Would you say that lung screening helps to save lives?
The only chance of a cure is to diagnose lung cancer as early as possible
Mathias Prokop
‘Well, it depends how you define saving lives. If you mean that patients do not die from lung cancer, then yes. The NELSON study showed that mortality among men decreased by 26% and among women even by 61%. Lung cancer screening appears to work better among female patients. This is probably because comorbidity amongst women is lower, and they more frequently have slow-growing tumours.
What is important is that, if we screen for long enough, the optimum effect on survival will develop. First data from the German LUSI (Lung Tumour Screening and Intervention Trial) confirms that the advanced tumour stages only disappear from about the third round of screening. It just takes a while until all tumours within the population have been captured and for new tumours to have been detected early enough.
Can we afford not to offer screening? Although life-extending treatment procedures for advanced tumour stages, such as immuno-therapy, work well, they are also very expensive and a significant burden for the healthcare system. The cost per life saved by a screening programme is therefore much lower. The only chance of a cure is to diagnose lung cancer as early as possible.’
Profile:
Radiology Professor Mathias Prokop heads the Department of Radiology and Nuclear Medicine at Radboud University Nijmegen, in the Netherlands. Over the last decade he has extensively researched chest screening with CT and he was significantly involved in the Dutch-Belgian lung cancer screening study (NELSON). He has been vice chairman of the Dutch Radiology Society and has repeatedly received awards from the Radiological Society of North America and the German Radiological Society.
24.10.2019