Article • The “invisible” population
Breast screening blind spot: Why transgender patients are falling through the cracks
Transgender patients are largely invisible in breast cancer screening statistics – and many never receive an invitation to participate in screening programmes. Guidelines exist, but awareness among referring physicians remains low. Experts say radiology departments are best positioned to lead the change by creating inclusive environments and actively reaching out to this underserved population. At the 2025 SBI Breast Imaging Symposium held in Colorado Springs, an expert outlined how imaging facilities can make a difference.
By Cynthia E. Keen

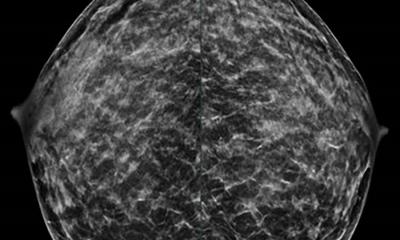
Image source: University of Rochester Medical Center
Do transgender individuals need regular breast cancer screening? Yes, some do. How many transgender women and men have had a breast cancer screening examination in the European Union? In the United Kingdom? In North America? What percentage of transgender patients need annual screening, based on well-established guidelines? The answers are simple. Nobody knows. Even in countries with near ubiquitous electronic health records (EHR) at hospitals and clinics, statistics don’t exist.
‘This population is so underserved it is invisible,’ Prof. Avice O’Connell, MD, of the University of Rochester, US, and a radiologist affiliated with Strong Memorial Hospital and Highland Hospital, told attendees at the 2025 SBI Breast Imaging Symposium held in Colorado Springs, Colorado.
The referral gap
Transfeminine patients living in countries which have national breast cancer screening programmes may not receive invitations to participate because they are registered by their sex assigned at birth. Transmasculine individuals who have genetic breast cancer risk factors and/or cisgender female breast tissue, but who are correctly identified as transgender males in EHR data, may be also excluded from invitations to participate in a national breast cancer screening programme. It’s a somewhat similar situation in the United States, where physicians make the referrals for breast imaging exams. But based on anecdotal observation of the small numbers of transgender patients getting screened, it is questionable if the referring physicians do so.
If you use the wrong terminology, you will lose trust. If patients feel comfortable, they will tell their friends who will start to come
Avice O’Connell
Data collection of mammograms performed on patients who identify themselves as transgender is not centralized and may not even be collected at imaging facilities where exams are being performed. In a world awash with data, information about breast cancer screening for and breast cancer developed by transgender patients is a series of not-even-guessable unknowns.
Dr. O’Connell suggested that hospital radiology departments and freestanding imaging centres are best positioned to change this. But first they must change to attract transgender patients who may be turned off by entering a “women’s imaging centre” or by encountering clinical and support staff who do not know inclusionary language or comfortable interaction strategy. ‘If you use the wrong terminology, you will lose trust,’ she cautioned. ‘If patients feel comfortable, they will tell their friends who will start to come.’
Creating an inclusive environment
Intake forms need to be gender neutral. Demographic data to be collected needs to include gender identity preference (male, female, or non-binary), as well as the sex assigned at birth. Patients should select the pronoun they relate to, and this preference should be used by radiology department staff.
It is essential that imaging facilities project a welcoming, neutral environment rather than a conventional feminine decor. This includes registration/check-in, colour of hospital gowns, changing areas, and screening and diagnostic waiting rooms. Signage in these areas needs to convey gender neutrality or inclusiveness. At least one clearly identified gender-neutral public restroom needs to be available.
Patients who are transgender should be advised of breast cancer screening guidelines, regardless of the type of imaging exam they are having.
Recommended article
Article • Overlooked and underserved populations
Breast imaging for male and transgender patients: bridging the knowledge gap
Breast imaging for male and transgender patients remains an under-researched field with significant gaps in guidelines and clinical practice. At the European Society of Breast Imaging (EUSOBI) annual scientific meeting, experts presented findings from a pan-European survey on male breast imaging and announced plans for a similar initiative focusing on transgender patients.
Guidelines exist – but awareness is low
Breast health and imaging experts from the American College of Radiology (ACR) published ACR Appropriateness Criteria® for Transgender Breast Cancer Screening in 2021.1 Guidelines with similar recommendations have also been published by a number of health organizations, including the World Professional Association of Transgender Health (WPATH),2 the University of California San Francisco (UCSF) Center of Excellence for Transgender Health, the Endocrine Society, and the American College of Obstetricians and Gynecologists.
This is important because a recent study conducted by the Mayo Clinic in Rochester, Minnesota, of its primary care and internal medicine physicians working at all Mayo Clinic locations, and those at the University of Michigan in Ann Arbor and the University of Texas - Medical Branch in Galveston, revealed that only 35% of the respondents were aware that breast cancer screening recommendations for transgender patients existed.3 Compounding this lack of awareness is concern by physicians about the accuracy and applicability of these guidelines because they reflect the best guess advice by experts, based on clinical analysis and studies of the data of cisgender women.
Anna D’Angelo, MD, a consultant radiologist at the Foundation Polyclinic University A. Gemelli in Rome, Italy, and a member of the European Society of Breast Imaging (EUSOBI) Young Club Committee, told AuntMinnie Europe in an interview, that the EUSOBI is planning to launch a survey among its members to collect data about the transgender population to identify areas that need improvement.4
Profile:
Avice M. O’Connell, MD, is professor of Imaging Sciences at the University of Rochester, New York, US. She is a breast screening expert with UR Medicine Breast Imaging. She received her medical degree from Trinity College, Dublin, Ireland. With over 30 years of experience in breast imaging, she is actively involved in teaching and research, with a particular focus on newer imaging modalities such as Cone-Beam Breast CT.
References:
- Expert Panel on Breast Imaging; Brown A, Lourenco AP, Niell BL, et al. “ACR Appropriateness Criteria® Transgender Breast Cancer Screening. J Am Coll Radiol. 2021;18(11S):S502-S515.
- Coleman E, Radix AE, Bouman WP, et al. “Standards of Care for the health of transgender and gender diverse people, Version 8.” Int J Transgend Health; 2022;23(Suppl1):S1-S259.
- Carroll EF, Woodard GA, St. Amand CM, et al. “Breast Cancer Screening Recommendations for Transgender and Gender Diverse Patients: A Knowledge and Familarity Assessment of Primary Care Practitioners.” J Community Health. 2023;48(5):889-897.
- Rylands-Monk F. “Transgender breast emerges as a priority for radiology.” AuntMinnie Europe.October 20, 2025.
10.02.2026