Article • Overlooked and underserved populations
Breast imaging for male and transgender patients: bridging the knowledge gap
Breast imaging for male and transgender patients remains an under-researched field with significant gaps in guidelines and clinical practice. At the European Society of Breast Imaging (EUSOBI) annual scientific meeting – held in Aberdeen, Scotland, in cooperation with the British Society of Breast Radiology – experts presented findings from a pan-European survey on male breast imaging and announced plans for a similar initiative focusing on transgender patients.
By Mark Nicholls

Photo courtesy of Prof. Healy
Professor Nuala Healy from the Beaumont Breast Centre in Dublin and the Royal College of Surgeons Ireland highlighted the absence of European guidelines for male breast imaging. 'Practitioners currently tend to follow the American College of Radiology and Royal College of Radiologists guidelines,' she explained. While only 5% of referrals to breast units are male, these patients generate a significant workload, with approximately 75% undergoing some form of imaging.
The majority of male breast disease is benign, ranging from lipoma to fat necrosis, gynecomastia and pseudo-gynecomastia. Male breast cancer accounts for just 1% of all breast cancers and 0.5% of all male cancers, generally presenting in older men.
Late diagnosis leads to worse outcomes
'Because male breast cancer is rare, there are very few prospective or randomised controlled trials in terms of treatment or management, so most of what we do with males with breast cancer is extrapolated from female breast cancer,' Healy continued. 'But about 40% of male breast cancers present at stage 3 or 4 at diagnosis and because they present later they tend to have much worse outcomes.' Risk factors include age, genetics – with BRCA2 more common in male breast cancer than in female – and anything that reduces testosterone or causes an increase in oestrogen.
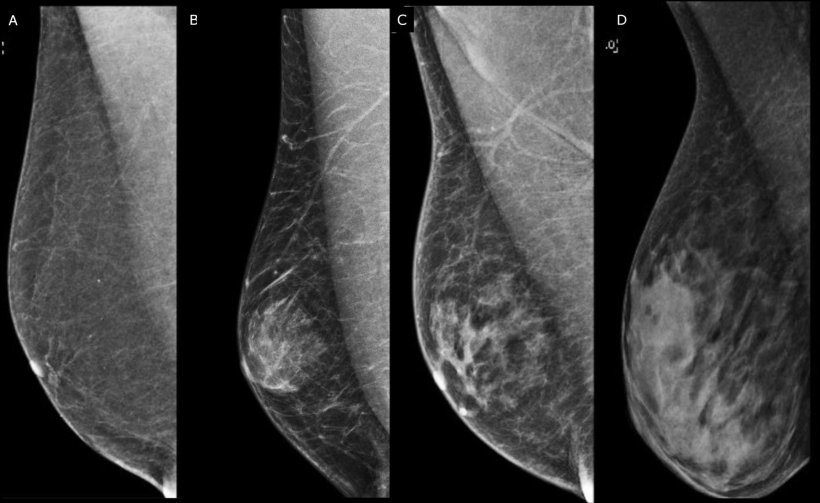
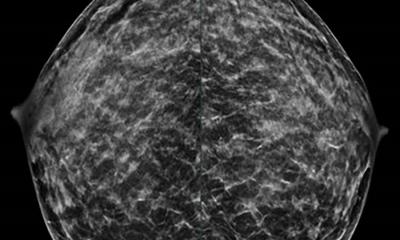
Image source: D’Angelo A, Portaluri A, Caprini F et al.: Male Breast: A Review of the Literature and Current State of the Art of Diagnostic Imaging Work-Up; Diagnostics 2023 (CC BY 4.0)
Pan-European survey maps imaging practices
The EUSOBI survey on male breast cancer was sent to breast imagers across Europe and received 825 responses – mostly from radiologists – across 34 countries. While the ACR and UK guidelines offer advice on use of ultrasound, mammograms or digital breast tomosynthesis (DBT) for men, survey respondents indicated varied approaches.
Many practitioners perform ultrasound for initial imaging in benign indeterminate palpable masses for men under 25, and mammogram or DBT for men over 50. For suspicious palpable masses, the vast majority (82%) use ultrasound for patients under 25 and a combination of mammogram or DBT for those over 50.
The survey also explored clinical approaches to gynecomastia and pseudo-gynecomastia. 'In younger populations, it is ultrasound and over 50 it is mammogram or DBT, while 72% of respondents said they did imaging for both unilateral and bilateral gynecomastia,' Healy reported.
In summary, most radiologists perform some form of imaging for gynecomastia, though 41% do not image males considered at high risk of breast cancer and 13% do not perform follow-up after a history of breast cancer. 'We need to do a lot more research in terms of male breast imaging and then develop some updated guidelines,' she concluded.
Transgender patients face multiple barriers

Image source: D’Angelo A, Portaluri A, Caprini F et al.: Male Breast: A Review of the Literature and Current State of the Art of Diagnostic Imaging Work-Up; Diagnostics 2023 (CC BY 4.0)
Anna D'Angelo from the Catholic University of the Sacred Heart in Rome addressed transgender breast imaging, emphasising the importance of correct terminology. Transgender, she clarified, is an umbrella term for people whose gender identity does not align with the sex assigned to them at birth, while cisgender describes people whose gender identity aligns with their birth-assigned sex.
D'Angelo focused on patients undergoing feminising and masculinising gender-affirming surgery and gender-affirming hormone therapy (GAHT). However, evidence of breast cancer risk in this population remains limited due to a lack of long-term follow-up, inadequate documentation of hormone exposure, and an absence of prospective studies.
Screening challenges and healthcare inequities
Breast cancer screening for transgender individuals faces multiple challenges, D'Angelo noted. These include low participation in or awareness of screening programmes, lack of trust in healthcare professionals, and poor knowledge of screening guidelines among both the transgender population and healthcare providers. A lack of training and education among clinicians compounds the problem.
'Radiologists must be familiar with the correct terminology and the types of gender-affirming processes; healthcare providers – both GPs and specialists – must be aware of the most current guidelines for the TGD population; the scientific societies and individual research groups must collaborate to close gaps in research and education, reducing healthcare inequities; and LGBTQIA+ advocacy groups should be involved in research and educational activities,' D'Angelo concluded. She confirmed that EUSOBI is launching a survey on radiologists' knowledge of transgender populations in breast imaging.
Dr Machteld Keupers from the University Hospital Leuven in Belgium discussed paediatric breast imaging, covering how to perform imaging in this age group, the most common benign and malignant breast lesions in children, and clinical management of paediatric breast masses.
Profiles:
Professor Nuala Healy is Chair of Radiology at RCSI University of Medicine and Health Sciences in Dublin, Ireland, where she leads the academic Department of Radiology while providing patient care as a consultant radiologist at Beaumont Hospital. She is the research lead for the British Society of Breast Radiology.
Anna D'Angelo is a radiologist at the Department of Radiology, Catholic University of the Sacred Heart and Fondazione Policlinico Universitario A. Gemelli IRCCS in Rome, Italy. Her research focuses on breast imaging, including neoadjuvant chemotherapy response assessment, automated breast ultrasound, MRI in breast cancer staging, and imaging in transgender populations. She has published extensively on ultrasound-guided biopsy techniques and radiomic applications in breast imaging.
Dr Machteld Keupers is a radiologist at the Department of Radiology, University Hospitals Leuven (UZ Leuven), Belgium, and is affiliated with the Department of Imaging and Pathology at KU Leuven. Her expertise includes breast imaging, mammography, digital breast tomosynthesis, and paediatric breast imaging. She has published research on breast imaging surveillance after curative treatment and is a regular faculty member at the Update in Breast Imaging conference.
10.12.2025