Breast screening in Belgium
Not so long ago this country, of considerable linguistic division, was a split into three regions, referred to as Flemish (with five provinces), Walloon (with five provinces) and the Brussels Capital. Each has its own parliament, with governments responsible for their individual region's affairs; these include health.
Dr Catherine Breucq, head of the Breast Imaging Department at Brussels University Hospital, is responsible for breast screening in two of the regions: Brussels Capital and Flemish. The latter has five reference centres (in four universities and the Bruges hospital). Each centre organises its own screenings, but all must follow the Belgian government's guidelines.
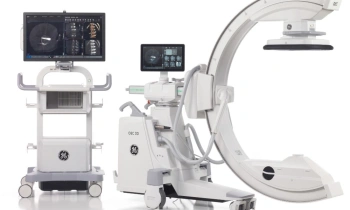
Meike Lerner spoke with Dr Breucq about a new and successful digital mammography project, the Mammobiel (Mammobile), which has begun to scan women in rural areas, who otherwise might not benefit from a screening programme. This unique unit was designed by the hospital with the help of Lamboo, a trailer company, and GE Healthcare, which equipped the truck with the digital mammography system Senographe Essential.

Prior to the launch of Belgium’s first digital Mammobiel, the country had two other mobile units. However, last year analogue equipment run by the University of Antwerp was put out of action, leaving one analogue system in service, still involving the procedure of image capture, film development, and so on.
The mobile breast screening project at Brussels University Hospital aimed to produce the most up-to-date Mammobiel, which, being digital, would provide greater performance and higher image quality specifically for dense breasts. This required in-depth planning, not only for scanner choice but also in consideration of the geographical elements of the rural areas to be served. As Dr Catherine Breucq pointed out, this country has many small, cobble-stone streets. ‘
We realised that the requirements to analogue and digital equipments in trailers are different. Because of digital detectors, digital equipment is more sensitive to shocks and also changes in temperature.
The chosen equipment is equipped with a detector that supports a wide range of temperature variation (15°C to 35°C), and the Lamboo trailer with the Senographe essential were tested at temperatures down to about -31°C +43°C-- they put it in a fridge,’ she said jokingly, recalling the degree to which the system had been tested. Along with shock resistance and temperature resistance, vibration was also an important element of those tests.
David Caumartin, general manager of GE Healthcare’s mammography business confirmed that this is ‘not a standard model’. The manufacturer, he explained, has helped produce other breast scanning mobile units, according to the needs of individual countries, and the type of vehicle and its layout. For example, in the Belgian mobile unit the trailer is 15x 3 metres; fitting it out involved input from radiographers, radiologists as well as a GE engineer. Another less critical factor, though nice all the same, was the choice of colour – pink – now so associated with breast cancer care and much accepted by women.
The entire system is built around the detector, the most important part of the image chain, he pointed out. ‘We build all the image chain ourselves and the technologies are different from others on the market, and means we can control their robustness for this type of usage. So, we know our detector is more reliable under stress conditions.’ ‘We also visited two or three Mammobiels last year,’ added Dr Breucq. ‘So it’s a growing process. But I think finally that, as a concept, we are not scoring too badly, and we’ve had many positive reactions. For us the most important thing was to reach a higher attendance rate. In some little villages, where there is no radiologist, and no private hospital, to get these women to attend mammography screening you must be there, and that’s with a nicely designed trailer, and high performance equipment.’
Another reason for the choice of the Senographe Essential was its considerable capacity, Dr Breucq pointed out. ‘If all the invited women arrive at the same time you have to do them, but if you have equipment where you lose time between two screenings (and there are a lot of companies that produce mammographs where you have a ghosting effect, it means you take a picture, for example, you turn the machine to have the oblique of the same side, then you must wait fifty seconds to a minute before taking another one, because the detector is memorising the previous image). This equipment works very, very quickly, without losing quality. That’s very important for us. If the patient is already in a good position, but the nurse has to wait between two screenings, that’s not a good system. For compression, this equipment also adapts to the shape of the breast, without pulling it. The less fear the patient has, the better she is positioned, the more relaxed she is and the better image you have, that’s the result.’
Women are invited for screening by the service, or can be invited by their general practitioners (GPs) or gynaecologists. ‘We started in the Flemish sector in 2001, with an initial attendance rate of less than 30%. The second round saw an increase of almost 12%. Now we have areas where attendance is above 50%. To meet the European guidelines you need 75% attendance. That’s very high, and it looks easy, but is not. In the Netherlands, for example, where they have been screening for 20 years, they have rates of 70-75%, but only after so many years. It’s a learning curve. Women have to know that there is cancer in life. It’s important to write about it because women have to be confronted about breast cancer. Every year in Belgium, October is breast cancer month. Well known people are helping us, for example actresses, and the Belgian singer Axelle Red, and Miss Belgium.’
The Mammobiel is manned by a nurse or radiographer and a secretary, who calculates the numbers in each area who are likely to arrive for scanning, and on that basis how long the unit should stay there.
As for numbers now being screened in the trailer, this much depends on the size of the villages visited. Theoretically, 15-18 women per hour could be scanned. In a small village, their stay may be two days. In the Flemish region, for example, in a village with 3,000 women residents almost 600 arrived in the market place for scans. However, in a city the trailer might stay for several days.
First and second readings are then carried out in the relevant hospitals, along with their own routine diagnostic examinations. If the first and second reading conflict, a third is undertaken. ‘If benign, we do nothing, even if you see a well-described cyst, you would not re-call the woman, because we are not searching for benign lesions, we are searching for cancers, malignant pathology.’ If malignancy is found, ultrasound follows, then possibly biopsy and MRI. The programme then re-calls the women in two ways. The referring doctor is sent a letter giving the results four days before the hospital sends another letter, this time to the patient. The doctor knows the result, but the patient is only told there is a problem, and she should come for a complementary examination. ‘We don’t talk about probably malignant, or malignant, because then 50% will never come. You have to decrease the fear.’
Dr Breucq then spoke of the need to follow the European guidelines, which ‘… means there is a level of quality not only in equipment but also in reading experience. If you perform 10 mammographies a month, you don’t have enough experience to detect a cancer in a second reading, so you cannot be a second reader.’ She also spoke of a significant problem in Brussels, where she is president of the screening organisation: ‘We have an attendance rate of 10%, not because the women don’t want to come, but because 45% are having diagnostic mammography. This means mammography and a radiologist decide whether -- ultrasound or a biopsy is necessary – making the cost double that of screening. In addition, very often in the 50-69 years group, where the breast is already fatty and you can see through it well, you don’t need an ultrasound, yet that is really the tendency of a few, elitist hospitals. In that way we will never increase participation in screening. There are several international studies, randomised trials that conclude that, with the 50-69 years group with a less dense breast, you are scoring perfectly with only mammography screening, for just 58 euros.’
Meike Lerner pointed out the advice of Professor Schulz-Wendtland (Germany) regarding multimodality diagnostics for breast cancer, i.e. first mammography, followed by ultrasound, biopsy, and then maybe MRI. Dr Breucq agreed with this sequence. ‘There was a time, two or three years ago, when MRI was really supported by several firms, and there were even patients who refused a mammography and wanted an MRI. I had to say: Sorry Miss, but with an MRI, I cannot assure you that you don’t have a non-invasive tumour. Okay, a big tumour, you will see it on an MRI, but you will also see it on an ultrasound -- for 18 Euros. An MRI scan costs almost 200 euros, so you have to see the cost and the benefit.
01.05.2009