Image source: Queen Mary University London
News • Tumour infiltrating lymphocyte measurement
Breast cancer: AI tool predicts which DCIS cases become invasive
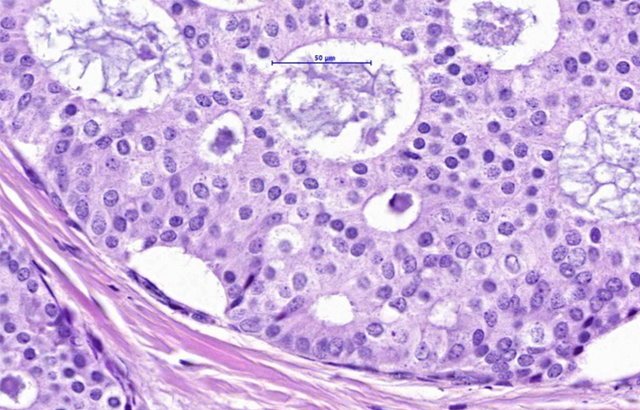
Researchers from Queen Mary University London and Emory University used a novel AI-based analytic tool to better understand how tumour infiltrating lymphocytes (TILs) can predict which cases of Ductal Carcinoma in Situ (DCIS) would go on to become invasive breast cancer.
DCIS is a form of early breast cancer, where some cells in the lining of ductal tissue have started to develop into cancer cells. Without treatment, a proportion of DCIS cases will go on to become invasive breast cancer.
The new study, published in Lancet Digital Health, is the largest and most robust investigation of automated estimation of these tumour infiltrating immune cells or TILs. Using randomised data from the UK/ANZ DCIS trial, researchers showed that a high density of TILs is associated with a 3-fold higher risk of progression to invasive breast cancer. Tumours with a high density of TILs were also found to be more susceptible to radiotherapy.
We have a robust biomarker that not only predicts which patients are at a substantially higher risk of progressing to invasive breast cancer but also tells us which subgroup of patients can avoid radiotherapy and thus help us prevent overtreatment
Mangesh Thorat
This work provides a new way to help distinguish and identify those women with DCIS who would benefit from radiation therapy over and above surgery from women who could be spared overtreatment in the form of radiation therapy. It could also be provided at lower cost to women with DCIS all over the world, thanks to its non-tissue destructive approach, which would allow more informed treatment decision making.
Senior co-author Mangesh Thorat, Honorary Reader, Wolfson Institute of Population Health, said: "We have done two key things here. Firstly, using the material from a randomised trial, we employed a very robust study design. This allowed us to eliminate limitations of previous studies and evaluate the biomarker in the best possible manner. Secondly, we harnessed the potential of AI to measure biomarker in a very precise quantitative manner, something humans cannot easily do. The result is that we have a robust biomarker that not only predicts which patients are at a substantially higher risk of progressing to invasive breast cancer but also tells us which subgroup of patients can avoid radiotherapy and thus help us prevent overtreatment."
This study was conducted by WIPH researchers with colleagues from Emory University, Atlanta, Georgia. The work was funded by Cancer Research UK, the US National Cancer Institute and the Breast Cancer Research Foundation, New York (NY, USA).
Source: Queen Mary University London
13.07.2024