News • Dermatology diagnostics
AI-powered app to speed up skin cancer diagnoses
Skin cancer is a particularly deceptive form of cancer. In the early stages, it looks very much like a harmless mole or birthmark and doesn’t cause any pain.
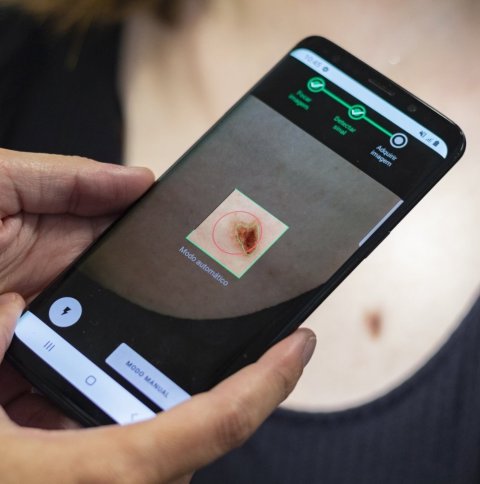
© Fraunhofer AICOS
According to data from the German Cancer Society, more than 200,000 people suffer from skin cancer every year in Germany. In 2017 alone, 3,764 people died from it. One of the most serious types of skin cancer is malignant melanoma, which is most frequently caused by exposure to the sun’s UV rays.
But, if caught in time, even melanoma is very likely to be cured. The survival rate is more than 95% after five years, which means that early diagnosis and prevention are even more crucial. The Fraunhofer Center for Assistive Information and Communication Solutions (AICOS) in Porto and Lisbon has developed a solution to accelerate early recognition. The Derm.AI solution combines smartphone photos of the skin lesion with image-analysis software and artificial intelligence. It provides a swift, first assessment of potentially dangerous changes in the surface of the skin. Dermatologists can access this decision support platform and analyze the cases with increased risk of skin cancer first. The Derm.AI solution aims to improve the existing Teledermatology processes in the Portuguese National Health System.
“In recent years, GPs have been increasingly concerned with spotting skin cancer early. People who notice dark spots or other perceptible changes to their skin need clarity quickly. But in regions with few specialists, it often takes a long time to get an appointment for the initial assessment. Often patients also have to travel long distances for these appointments, too. This is where our Derm.AI solution comes in,” says Maria Vasconcelos, Senior Scientist at Fraunhofer AICOS.
Recommended article

Article • Skin cancer identification
Dermatology & AI: The need to quantify skin tones
Although artificial intelligence (AI) tools and smartphone apps that help identify suspicious moles and potential skin cancers are starting to proliferate, dermatology informatics has far to go before becoming a clinically adoptable technology. Many challenges need to be resolved, not least of which is the need for more image data representing people of colour.
The first step is for the GP to photograph the potential problem area on the skin with a smartphone. The Fraunhofer team developed a special app just for this purpose that runs on both iPhones and Android smartphones. The app ensures that the photos are correctly aligned, taken at the right distance and have the correct resolution. The app takes two photos: one close-up of the suspicious area and one from further away to show the area in context. It also helps to correctly align and position the camera. This creates standardized photos with consistent settings for resolution, color, brightness and contrast. “The standardized shots are easy to compare and can be reliably analyzed by specialists,” Vasconcelos explains.
We had a lot of discussions with GP and dermatologists to really understand what they need
Maria Vasconcelos
The images obtained at the GP’s practice are then sent via the internet to the dermatology department of a hospital. This is where the artificial intelligence software comes into play. It analyzes the photos of the skin lesion, compares them to reference data and the data of other patients and provides a risk assessment. The lesion in question is labeled as “normal”, “priority” or “high priority.” This is not yet a formal diagnosis, it is simply a first assessment which helps prioritize the order in which the potential cases are examined. The doctors can prioritize examining the cases which the AI software has indicated have a high risk, as these need to be quickly confirmed or clarified. “The software doesn’t make a decision; it simply provides a pre-selection based on probability. The actual examination and diagnosis are still in the hands of the dermatologists or skin-cancer specialists,” Vasconcelos explains. After the images are analyzed, along with the patient data such as age, gender or previous conditions, the dermatologist at the hospital can either provide feedback to the GP responsible for the patient via teleconsultation or schedule a presential consultation with the patient.
In more dubious cases regarding the risk level of the skin lesion, the dermatological specialists book an in-person appointment. In this appointment, they will, for example, examine the patch of skin under a reflected-light microscope or take tissue samples for analysis by means of biopsy.
Around 80% of the cases in which patients present themselves at the GP’s practice with a suspicious change in their skin prove to be harmless moles or birthmarks, after image analysis and consultation between the doctor and the dermatologist. This enables GPs to quickly give patients the all-clear, saving them long periods of waiting and an often-long journey to a hospital appointment. For patients whose skin changes are not clearly identifiable as harmless or for those which indicate a less dangerous form of skin cancer, the GP asks the patient to return, for example in three months, and have another photo taken of the area.
During the Derm.AI project, the AICOS researcher and her team developed the algorithm for the image-analysis software. The deep-learning software was fed with image data and information from around 4000 cases. The algorithm also utilized the expert knowledge of dermatologists in the subsequent prioritization. “We had a lot of discussions with GP and dermatologists to really understand what they need. We have received very good feedback from doctors for Derm.AI,” Vasconcelos is pleased to announce.
Source: Fraunhofer Center for Assistive Information and Communication Solutions (AICOS)
02.02.2022