Advances in blood group serology
Todays test formats (gel technology, micro test plates), plus laboratory electronic data processing and automation, have changed the classic format of blood group serological examinations significantly - and reduced the danger of life-threatening errors.

However, the degree of automation for blood group serological patient diagnoses, in hospitals or in prenatal diagnostics, has not kept pace. In the recently published annual ‘Serious Hazards of Transfusion (SHOT) report covering 2000-2001, 92% of English hospitals reported incidents or near-incidents during transfusions. 315 incidents were registered as occurring during ransfusions. In 213 of these, the wrong blood type had been transfused. In 14% of these cases this related to incompatibility of blood group AB0. In 10% it was intolerance of the Rhesus factor Rh(D). The transfusion of incompatible blood in the AB0 group led to one death and severe follow-on illness in three cases due to intravasal haemolysis.
Over five years, the SHOT analysis found that during 699 transfusion incidents, 11 patients died and another 60 became so ill that they were admitted to intensive care units (ICUs).
The SHOT report reveals that about 30% of mistakes and reasons for transfusion incidents emanated from hospital laboratories. Interestingly, over a third of mistakes occurred outside the labs’ routine hours, an observation that questions the experience of night and weekend staff to ensure technically faultless implementation of testing and interpretation of results.
Analysis of mistakes shows that, within blood group serology (typing, antibody diagnosis, compatibility examinations), the reasons for the errors were very different.
In blood typing (AB0, Rh(D)) in most cases it was not the choice of reagents or technical procedures that led to the wrong results; it was unsuitable laboratory organisation (necessary controls not being performed, no cross-checks with previous results). The reasons for mistakes in antibody diagnoses (antibody search and identification) are more varied. This involved both unsuitable laboratory organisation, the fact that methods that were not sufficiently sensitive - such as those used to diagnose clinically relevant Kidd antibodies - and the technical failure of reagents, which led to transfusion incidents.
The SHOT analysis also shows that the error rate during mass blood donations is very low. According to the authors, a carefully implemented quality management system (comprehensive validation of processes) and full automation of tests, including documentation, helped to lower error rates significantly.
As only 35% of English hospitals reported (2000) that they had automated their blood group serological examinations, the SHOT analysis concludes that the implementation of full automation could reduce the incidence of human error in hospital laboratories significantly.
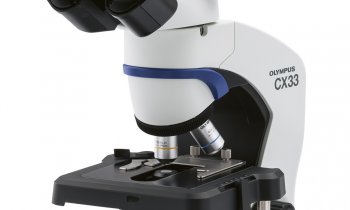
Recent developments in equipment and technology not only fulfil requirements for more safety and certainty in testing and documentation, but they also meet the special standards required in hospitals.
These include:
• The highest level of flexibility through random access. With patient diagnostics in hospitals, unlike with donor diagnostics, it is not normally possible to combine individual samples into large test series; moreover, test profiles in hospital patient diagnostics are normally much more comprehensive and more heterogeneous.
• In daily hospital routine it is important that quick testing of emergency samples is given the highest priority and that full automation is constantly available, so that results can be achieved quickly even when there are staff shortages or lack of staff outside routine working hours.
• The presence of long-term storage of patient data and results, for comparison of new and old results and to check for discrepancies, as well as communication with IT systems, enhance the suitability of automation concepts for hospitals and, in future, will help to reduce the number of transfusion incidents.
Outlook - Whist molecular-biological methods for routine typing are increasingly used in transplant diagnostics and other medical fields - with serological methods moving into the background - classical methods, such as agglutination or solid phase techniques combined with automated solutions, will continue to play an important role in routine blood group serology. Molecular biological methods or chip technology will only be of significance for very specific examinations such as determination of very weak Rhesus-D features to D-partial antigens, within the area of donor and prenatal diagnostics in forensic medicine.
30.04.2003