Prostate pathological
A pathologist’s view of prostate diagnostics
Pathology is the gold standard of prostate diagnostics. Whilst the radiologist makes interpretations based on shadows and grey scale values visible on an image, the pathologist has the ‘fait accompli’ under the microscope. Professor Glen Kristiansen, Director at the Institute for Pathology at the University Hospital Bonn, explains why image-guided biopsies also make sense from the pathologist’s point of view and why the prognosis for prostate cancer is a special case.
Report: Karoline Laarmann

No pathologist in Germany has published as many scientific works on the topic of prostate cancer as Glen Kristiansen. He believes that a qualified specialisation in specific organs, as is common in the USA, makes sense, but that it cannot be realised in Germany: ‘There is an increasing lack of qualified staff in pathology. When we look at how many pathologists per residents Germany has, we’re in third place from the bottom, ahead only of Turkey and Poland. The situation is bound to get worse over the next few years as our field suffers from aging, recruitment problems and, to make matters worse, from requirements planning.’
Kristiansen specifically welcomes advances in imaging because these developments also lead to reduced workloads in pathology. He approves of the demand for image-guided prostate biopsies: ‘In every other case seen by pathologists the tissue sample is negative. However, we obviously never know whether the patient really is free of cancer or whether the biopsy was taken “blind” from the wrong area. This is like playing Battleship.’
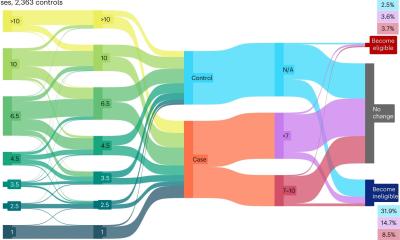
The International Society of Urological Pathology introduced one important advance, from the pathologist’s viewpoint, in November 2014. The Gleason-Score, i.e. information about the growth pattern, and therefore aggressiveness of a prostate cancer, was divided into five prognostic groups. Kristiansen explains why this is so important: ‘Most patients with prostate cancer are already of an advanced age. At the same time this cancer grows very slowly. So, the question is: Will the patient actually be alive for long enough to benefit from treatment or not?’ This group division helps to advise patients in a forward-looking manner.
Over the last decades there have already been several shifts in paradigm regarding the prostate cancer treatment, the pathologist notes. ‘In the 1980s prostate cancer was still treated as some form of ‘senile wart’ occurring in men. The motto was: You die with prostate cancer but not because of prostate cancer. Therefore, it mostly wasn’t even treated. However, the available data has shown that there definitely are patients who die from this cancer. The pendulum swing then changed direction and the strategy was to find and treat as many cases of prostate cancer as possible.’
Although surgery and radiotherapy are treatment options, they are not without risks and side effects. A prostatectomy for instance can lead to incontinence and problems with potency and can therefore limit a patient’s quality of life significantly.
The high prognostic significance of the Gleason-Score has turned it into an important parameter for treatment planning, but the problem of tumour heterogeneity remains – despite multiple, blind biopsies, as the aggressiveness of a cancer can be very different in different parts of a tumour. In this context the pathologist emphasises once more: ‘If we had image-guided prostate biopsies we could hold better, pre-therapeutic case conferences, where radiologists can present the information gained from images and pathologists could present their diagnostic findings gained from tissue analyses. ‘Both disciplines would benefit from this, but most importantly so would the patient.’
PROFILE:
Glen Kristiansen was Professor for Molecular Tumour Pathology and Senior Consultant of the Pathology Department, University of Zurich for four years before he took over the directorship of the Institute for Pathology at Bonn University Hospital in May 2011. The pathologist is a Member of the Board and European Representative of the International Society of Urological Pathology (ISUP) and of the Advisory Board at the European Network for Uropathology (ENUP). He is also a member of the WHO Panel of Experts on Urological Pathology and of numerous other national and international specialist pathology- and cancer research associations.
08.07.2015