Article • Interventional Radiology
3-D simulation includes haemodynamics
New 3-D simulation models that include haemodynamics enable better treatment of hepatic tumours via radio-embolisation, according to eminent Spanish radiologist José Ignacio Bilbao Jaureguizar.
Report: Mélisande Rouger

In radio-embolisation, an endovascular technique currently used almost exclusively in liver cancer therapy, particles are liberated in the arterial flow of a vessel feeding hepatic tumours, to deploy the particles within the arterial tumoural network.
Interventional radiologists use a microcatheter through which they inject particles loaded with yttrium-90, which emit radiation in a diameter between 2.5 and 11 mm for about 64 hours.
Crucially, the particles must be placed within the tumour, so that the total radiation goes only there. However, doing so remains a challenging exercise, mainly due to the blood stream.
Depending on the arterial flow, areas of the tumour may receive more or less particles, according to José Ignacio Bilbao Jaureguizar, professor of radiology, head of interventional radiology and consultant radiologist at University Clinic of Navarre in Pamplona, Spain.
‘This is one of the problems we have,’ he explained. ‘We use angiography and selective catheterisation techniques to homogenously distribute the particles, but it all depends on blood flow in the end. So some areas will be treated appropriately, and others won’t – or not as much.’
There are many parameters to factor in and countless scenarios in which particle distribution is not as homogenous as it should be:
José Ignacio Bilbao
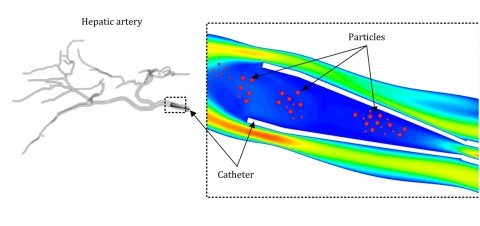
Because they needed to understand vascular flows better, Bilbao’s department decided to team up with the University of Navarre (UN) School of Engineering in neighbouring San Sebastian, to help develop a computational simulation model based on the anatomy, to study all possible scenarios of particles distribution. (See: Numerical investigation of liver radio-embolisation via computational).
The simulation model takes into account all the available information, such as what kind of catheter will be used and its shape, or its distance from the next arterial bifurcation.
‘There are many parameters to factor in and countless scenarios in which particle distribution is not as homogenous as it should be,’ Bilbao explained. ‘For example, if you place a catheter close to the bifurcation of two arteries that have the same calibre, you might wrongly assume that 50% of the particles would go left and 50% right. But blood stream is a complex physiological process, and a catheter, even if only a 1mm calibre, may interfere with it,’ he said. ‘You may also obtain different results if you place the tip of the catheter close or further to the bifurcation, in a central or lateral position in the vessel, or if you liberate particles at high or low speed.’
The UN researchers came up with a large amount of possibilities and findings using and analysing real-sized 3-D models, according to Bilbao, who compared particles distribution to cars in highway traffic. ‘We are learning a tremendous set of things. Simulation models enable us to test new catheters and see if they work, or not, understand how our equipment works, and issue appropriate user recommendations, among others. It opens up a lot of possibilities.’
Radiology began to take an interest in haemodynamics study a few years ago, when a team in the USA showed the value of studying blood flow in prosthesis placing to correct aneurysms in the aorta (Basciano CA. Computational particle-haemodynamics analysis applied to an abdominal aortic aneurysm with thrombus and microsphere-targeting of liver tumours. PhD Thesis, North Carolina State University, Raleigh, NC, 2010.)
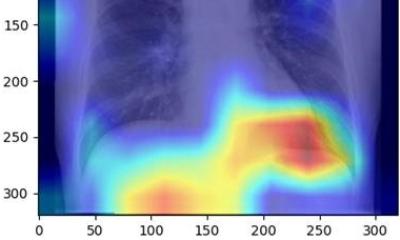
Studying smaller mobile vessels in the liver is just as interesting an option for radiologists, but they must learn to focus on functional imaging, Bilbao believes. ‘We can’t work with morphological criteria alone any more; we need function. Radiology is a wonderful morphological technique and we’re particularly fond of studying microanatomy in depth. However we must get involved in function and find out more about fluid dynamics.’
In the future, 3-D simulation models should be tailored to every patient. This would prove of tremendous help in brain cancer surgery for instance, Bilbao added. ’We still have a lot of work ahead. Developing a simulation model takes thousands of hours on a super computer. It’s not only about money, but also techniques. It could take years, but things go so fast now, so who knows?
Profile:
José Ignacio Bilbao Jaureguizar is professor of radiology, head of interventional radiology and consultant radiologist at University Clinic of Navarre (UCN) in Pamplona, Spain. He is also former chairman of UCN radiology department. He gained a medical degree at Navarre University’s medical faculty. Training followed in interventional radiology at MD Anderson Cancer Centre, Houston, USA and he received his PhD, cum laude, at Navarre University. His research interests are percutaneous treatment of tumours including chemotherapy and embolisation, especially in liver tumours.
03.03.2017