Video • Epidemiologist Q&A
12 things you should know about the new coronavirus
The novel coronavirus that recently originated in Wuhan, China has grabbed headlines and caused concern among public health officials around the world.
Two infectious disease experts—Professor of Medicine Peter Axelrod, an infectious disease specialist at Temple University Hospital, and Assistant Professor of Epidemiology Krys Johnson, an epidemiologist and instructor in the College of Public Health—share their insights on the novel coronavirus epidemic.
Q: What is a coronavirus, and what are some characteristics that make this particular coronavirus—2019-nCoV, the Wuhan coronavirus—different from others?
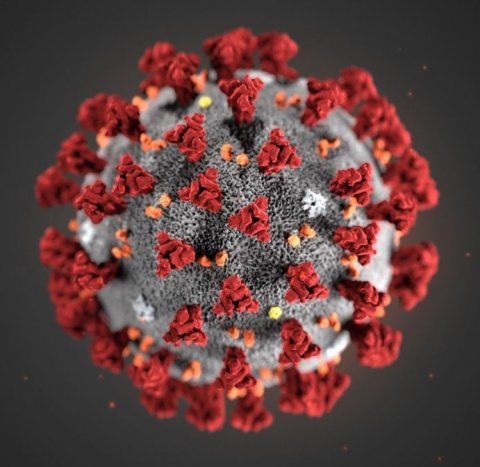
Image source: Centers for Disease Control and Prevention (CDC)/Alissa Eckert, MS
Axelrod: Coronaviruses are common community-acquired respiratory viruses, and their manifestations really range from a mild cold to a severe pneumonia. There are some strains that seem to be particularly likely to cause severe respiratory infections, such as the strain several years ago in the Middle East called Middle East respiratory syndrome (MERS), SARS, or severe acute respiratory syndrome, in the early 2000s in China. They were both coronaviruses, but we mostly see these viruses as causing a cold. This particular virus, we know, is genetically different from other coronaviruses that have been discovered in the past. Researchers have been able to sequence the RNA of the entire virus, so they know that it’s different. It seems to be not as severe as the SARS coronavirus, at least so far.
Johnson: A coronavirus simply is a type of virus. We have multiple viruses that we deal with all the time. We’re very familiar with influenza virus, for example, and with that, we know there are different strains of it, and the coronavirus is just that way, there are different strains of it, and they comprise things like the common cold or MERS or SARS. We hear about MERS and SARS more often because people die from them more often. But if we actually compare them to influenza, more people die of influenza every year than any of these—MERS, SARS or other major coronaviruses.
Q: We’ve heard a lot about the market in Wuhan, China where this virus is suspected to have originated. Where do these viruses come from, and how do they spread from animals to humans?
Johnson: We think that they come from an animal reservoir, which means that they infect animals, and whenever they’re trying to replicate, they typically replicate just in an animal and are passed from animal to animal and usually don’t make the jump to humans. But when they do, it can be because someone is consuming infected meat that hasn’t been prepared properly. It could also be that in the process of butchering, that someone has a cut, and that becomes infected with bodily fluids from one of those infected animals. Either of those can be a potential way for that virus to make the jump from an animal to a human, and it’s not particularly uncommon. Those are actually called zoonotic diseases, and that just means that humans can get them from animals.
Recommended article

Interview • Infection control
Virologists are today’s universal necessities
Globalisation has been a defining term in this 21st century: with almost anybody able to visit any place at any time, diseases, viruses and bacteria can be travel companions. Thus virology is gaining increased attention. Professor Barbara Gärtner, President of the German Association of Virology, talks about the issues and challenges arising from this development.
Q: What are the main symptoms of this coronavirus?
Axelrod: From what we know, it seems like the main hallmarks are fever and respiratory symptoms—mostly cough, shortness of breath, chest pain. It can be very similar to the flu, but the cough and shortness of breath are more prominent.
Q: What can people do to avoid getting sick, with a coronavirus or any other illness?
Johnson: If you want to reduce the likelihood of getting coronavirus, you would do the same thing that you would do to prevent getting the flu. Make sure you wash your hands as often as you can, use an alcohol-based hand sanitizer—they have found the coronavirus does die in the presence of an alcohol-based hand sanitizer, so that’s a good thing to keep on your person at all times, especially if you use a train or a bus and you don’t really have access to washing your hands. Make sure that if you’re sneezing, you’re sneezing into your arm so you’re not putting droplets out into the atmosphere, and if someone sneezes or coughs around you, just try to be very cognizant of that and make sure you’re not breathing in anything that they could’ve just coughed up.
Q: Where can people find reliable information about the coronavirus epidemic?
Johnson: I would recommend people go to the same information sites that epidemiologists, public health workers and clinicians use. We use the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) as our go-to sites to see what the new information is for any disease, but especially for novel diseases like this coronavirus. The CDC updates their website regularly, so they’ve been good about making sure that we get the most up to date information about coronavirus about how it transmits and how infectious it is.
Q: How are cases or suspected cases of this new coronavirus identified and differentiated from other similar illnesses, like the flu?
Axelrod: One thing we don’t really know a lot about yet is the mild cases, so if somebody has a sore throat and a little bit of a cough and doesn’t feel that sick, could this be the new coronavirus or not? We may only be seeing the more extreme end of it, because people with more mild illness aren’t seeking medical care.
With the flu, you often get severe muscle aches and headaches; with this coronavirus, evidence suggests shortness of breath develops in 55 percent of cases after about a week. That’s not like the flu—with the flu, you rarely would be short of breath.
In the U.S., the flu is way more common, so really the main clue would be a travel history. So far, all the U.S. cases have come in people who have traveled to China. But if there starts to be secondary transmission, it gets trickier.
Recommended article
Video • New virus 2019-nCoV
Scientists grow Wuhan coronavirus in the lab
Scientists from The Peter Doherty Institute for Infection and Immunity in Melbourne have successfully grown the Wuhan coronavirus (also known as SARS-CoV-2) from a patient sample, which will provide expert international laboratories with crucial information to help combat the virus. This is the first time the virus has been grown in cell culture outside of China. The Royal Melbourne Hospital’s…
Q: How does the lab test to identify this new coronavirus, work, and why is it taking some time to confirm or rule out cases?
Axelrod: They’re basically looking for the viral RNA, and it’s kind of like a jigsaw puzzle. If you’re putting together a jigsaw puzzle and your piece doesn’t fit, you can’t make it fit, but if your piece fits exactly, it slides right in. Tools to find RNA are like that. It has enough of a pattern to it so not just any virus can slide right in; it has to be the right sequence.
It can be done fairly quickly within a couple hours, as opposed to a cell culture, which takes days—but right now, the materials available to test for this coronavirus are only available at the CDC. They’re trying to make it available at state labs, but it isn’t yet, so the CDC was sort of bombarded with requests for testing. Labs that are set up to do PCR testing can handle a lot of samples, but all of the materials have to be made ready for the specific virus being tested. But it’s not instantaneous.
Q: What’s the relationship between this virus and pneumonia?
Axelrod: Pneumonia really just means an infection of the air spaces of the lung. When I talk to medical students, I tell them to imagine a sponge. The sponge has little tiny air spaces all within it, that’s kind of what the tissue of the lung is like. If that sponge was put under water, now all of a sudden all those little holes are filled with water, and if that fluid is infected, it’s pneumonia.
Q: Should people in the Philadelphia region or the United States in general be concerned at this point?
The important thing to remember about this coronavirus is that we’re mainly concerned because we don’t know that much about it, but really, the flu impacts a lot more people
Krys Johnson
Axelrod: No. Influenza is, at this moment, way more concerning here, so if you’re worried about getting sick, I would say get a flu shot. If you drive in your car, buckle your seatbelt, because that’s way more likely to be important than worrying about coronavirus.
Johnson: The important thing to remember about this coronavirus is that we’re mainly concerned because we don’t know that much about it, but really, the flu impacts a lot more people. Hundreds of thousands of people in the United States get the flu every year, and thousands of people here die from it. No one yet in the United States or Canada has died from the coronavirus, because we have accessible supportive therapies. It’s important to make sure that you’re getting your flu vaccine, and also important to make sure you’re taking precautions so that you don’t come into contact with any respiratory illness.
Q: The CDC has issued a travel advisory recommending that people avoid non-essential travel to China during this epidemic. What does this mean, and how common is this?
Johnson: The CDC issues these travel advisories pretty much every time there is an epidemic, so when we had the Ebola epidemic in western Africa, there was a travel advisory for that area. When MERS was an issue in Saudi Arabia, there was a travel advisory issued there. So these are very commonplace, and they’re meant to be preventative. And if people need to travel there anyway, they just need to be very cognizant of their personal hygiene and making sure they’re being proactive in preventing the likelihood of being infected by those illnesses. MERS, SARS and the current coronavirus all share that they were most often communicated person-to-person in very population dense areas. As long as people are taking care of themselves, making sure if they’re symptomatic, that they’re staying home, so if you have a fever, if you have chills, whether it’s the flu or coronavirus, you should stay home and take care of yourself. If you have any likelihood of having this actual coronavirus, you should call your physician before you go in just to make sure they’re taking the appropriate precautions for themselves and for other patients who may be in the waiting room.
Q: How contagious is this particular virus?
Axelrod: It’s likely spread in a fashion similar to rhinoviruses, which cause most common colds—via direct contact with secretions or large droplets (such as from a cough or sneeze of someone close by). So not like measles, where tiny droplets can spread for yards and infect people. If a virus mostly lives in large droplets, usually you have to be within three feet of a person who’s coughing to be at risk. On the other hand, if it lived in tiny droplets like measles does, then you can be pretty far away and still breathe it in.
Q: What should we expect to see happen with this virus in the coming weeks and months?
Axelrod: We’ll have to see what happens with worldwide transmission over the next two to three months to determine if it’s going to be a commonplace concern or not. We just don’t know that yet.
Johnson: In the coming weeks and months, we should expect to see information evolve. So just in the last week, we have had a lot of differing opinions on how infectious this disease is, and that’s just how epidemics go. As we learn more, we revise what we’ve learned. With Zika virus, we had new guidance from CDC every Friday. I would expect us to see no less for the coronavirus, and they actually seem to be updating guidance for the coronavirus more frequently, as I said, they updated it just yesterday, and they’re likely to update it again today. So just making sure that we continually check those websites to see what’s changing, and making sure that we’re going to media that are reputable in citing these scientific journals and not awfulizing the situation, because I do not think that there is a need for panic. Like I said, we deal with coronaviruses every day; most of us have it before we’re a year old, so it’s just a matter of protecting ourselves as we would from any other disease.
Source: Temple University
06.02.2020