When rejection comes from within
A new cellular structure responsible for previously unexplained rejection of organ transplants has been identified by researchers at the University of Montreal Hospital Research Centre (CRCHUM.)
This discovery could one day revolutionize transplantation practice by modifying risk assessment of rejection in people who receive heart, lung, kidney, or liver transplants. "We have found the mechanism that makes patients react against components of their own blood vessels even before receiving an organ transplant, and we have identified a drug that can prevent this type of rejection," said Dr. Marie-Josée Hébert, a transplant physician and researcher at the CRCHUM and a professor at the university's Department of Medicine. The findings were published today in Science Translational Medicine
Rejection is a risk of transplantation. The phenomenon is usually caused by a reaction of the recipient's immune system vis-à-vis the transplant, which it considers an invader. HLAs (human leucocyte antigens), which are present on the surface of all cells, are a sort of unique identifier for each person. In transplants, doctors try to avoid rejection by ensuring that the donor and recipient are compatible with regard to blood group and HLA antigens. Despite these precautions, one in ten transplants results in rejection.
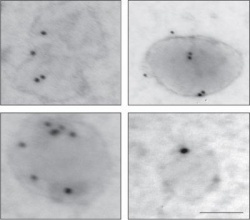
To solve this mystery, the researchers focused on blood vessels, an important component in transplantation. When blood vessels are damaged, rejection is more difficult to treat. "We discovered that the damaged blood vessels release specific bits of cells: small membrane vesicles that put the immune system on alert. If we then perform a transplant, the immune system immediately attacks the donor organ," said Melanie Dieudé, a researcher at the CRCHUM and first author of the study.
The tiny vesicles derive from dying cells and produce autoantibodies. "In addition to the immune system reacting against HLAs, it surprisingly reacts against components of our own cells. So rejection is not simply a reaction against another person, it is also a reaction against elements that belong to us," said Dr. Hébert, who is also Co-director of the Canadian National Transplant Research Program.
Hébert's team has found a way to neutralize the enzyme driver of these small vesicles, the proteasome, through a drug currently used to treat certain cancers of the bone marrow, bortezomib. The drug acts by blocking the enzyme activity of the vesicles, which has the effect of making the immune system deaf to alerts. Results from cultured cells and animal models are promising, and a clinical study in humans is ongoing. "If a recipient has already reacted to these small vesicles and receives an organ that is also in the process of releasing vesicles, it is probably a dangerous situation. This is what we are still examining," explained Hébert. Since the first organ transplant in 1954 by Dr. Joseph Murray in Boston, transplants have improved. Research on the compatibility of blood groups and HLA antigens before transplantation, and the development of treatments to combat rejection, such as corticosteroids, x-rays, and immunosuppressants, have enabled doctors to perform transplants that have saved lives. This latest discovery could help save more. "It is still too early to consider changing clinical guidelines, but I think it could one day change how organs are allocated for transplants. Organ recipients could also be treated before the operation to make them more silent to these signals coming from ourselves," concluded Hébert.
Source: University of Montreal Hospital Research Centre (CRCHUM)
18.12.2015