Zero percent and other illusions
Professor Tobias Welte MD, President of the 24th International Congress of the European Respiratory Society, gave EH some personal views on the symposium ‘New perspectives in the management of nosocomial pneumonia’.
Interview: Ralf Mateblowski

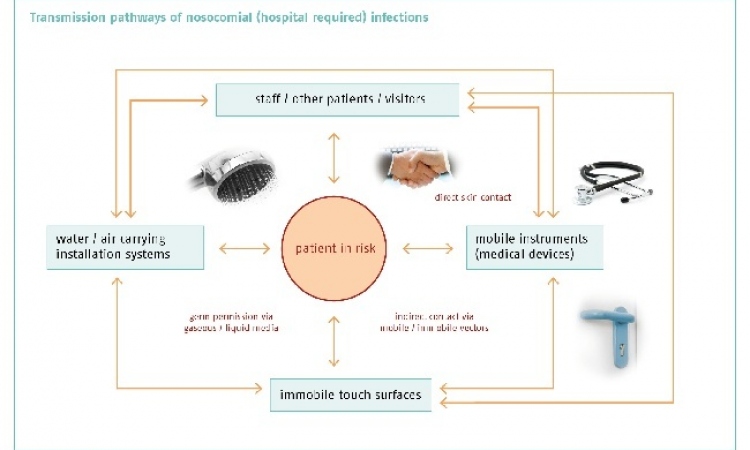
‘A load of nonsense!’ Such was the professor’s spontaneous response to calls for complete avoidance of nosocomial infections. ‘You always have to differentiate between nosocomial infections that are acquired and those which come from patients themselves,’ he explained. ‘When patients suffering chronic colonisation with nosocomial pathogens in the bowel have to undergo abdominal surgery then infections sometimes simply cannot be avoided - and the majority of all infections are based on this endogenous, intrinsic mechanism. It is therefore an illusion to believe nosocomial infections can be entirely avoided. On the contrary: The majority cannot be avoided!’
Nevertheless, there are noteworthy successes in prevention. ‘For a long time the focus was on MRSA; ten years ago we had an increasing prevalence in Germany of 22-25%. Since then, we have seen a slight drop to currently around 17-20% because of more standardised infection prevention and control procedures. A further decrease is possible, but it would be an illusion to believe that the figure can be cut to below 10%.’
The main reason for this is that staphylococcus bacteria are different from other pathogens in their biology and disease mechanisms. ‘Resistant coli, for instance, are almost never transmitted via the hands but, in the case of staphylococcus, hand hygiene is the key issue! The clean hands campaign, supported by the Federal Ministry of Health, was very successful. Standards were developed for many procedures where staphylococcal infections play a part, such as for inserting catheters.
It’s all the more incomprehensible then that the coordinating manager of the national reference centre, Professor Gastmeier, is currently having to look for private sponsors because the federal government no longer finances this campaign!’
The symposium in Munich also featured discussions about HAP (hospital acquired pneumonia) and the American programme ‘zero VAP’, aimed at reducing the number of ventilator associated pneumonia cases to zero. Says Welte: ‘The Americans have now realised that this measure is absurd: with a patho-mechanism that causes such complex cases of pneumonia you can only influence some individual factors, but not patient-inherent ones. As yet, there are no significant procedures for this.’
A lot has been invested over the last few years to accelerate infection diagnosis. This has two major implications, says the pulmonologist: ‘The classic, microbiological diagnosis has become much faster; resistant pathogens can now be isolated and identified in just a day.
Additionally, modern PCR systems help to gain another few hours. However, the disadvantage is that these staff and equipment intensive procedures are based on amplification, meaning they can only detect what is coded on the chip.
‘That’s easier for gram-positive pathogens with their fairly preserved, standard resistance mechanisms, than for gram-negative pathogens, where we basically observe new resistance mechanisms emerge almost every week. In my view it will be hard for PCR procedures to become established in the hospital. There also will be no way around classic microbiology in the future.’
Could the rise in resistances be contained? Welte is optimistic: ‘Thankfully there is finally a little more happening with regards to the development of new substances. At the beginning of October a new cephalosporin* was introduced to the German market that’s also effective against MRSA. Some other substances are also currently going through the licensing procedures, so we should be able to move on from the very low point – i.e. 10 years without new antibiotics.
‘However, the problem remains that the development of resistances occurs much faster than that of the new substances. Too many factors come into play here, including the misuse of antibiotics itself, their widespread use in mass farming and the globalisation of resistances through tourism.
‘Ultimately, the much-needed support from politicians is not forthcoming: All (preventative) measures are labour-intensive. In high-risk areas, such as intensive care units, the staff cover in many places is already insufficient. If staff numbers keep being reduced further for economic reasons all well-meant infection prevention and control programmes will be of no benefit – and incidentally, neither are standards and guidelines implemented on their own, without repetitive teaching and monitoring!’
* A group of broad-spectrum antibiotics that prevent the rebuilding of the cell walls in bacteria that divide and therefore have a bactericidal effect. Penicillin falls within this group.
PROFILE:
Tobias Welte MD is a specialist in internal medicine, pulmonology, critical care and infectology. Early on in his career he was a house officer and registrar in Lehrte and Hanover, before spending a decade as head of the Pulmonology and Critical Care Medicine Division, at Otto-von-Guericke University, Magdeburg. The professor has directed the Department of Pulmonology at Hannover Medical School since 2004 and is the current president of the German Respiratory Society.
30.10.2014