Worldwide about 600,000 new cases of breast cancer are diagnosed annually
Screening update
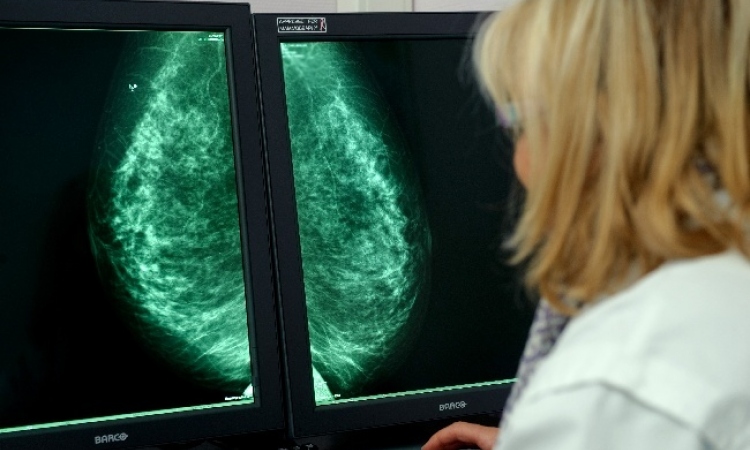
Mammography plays a critical part in diagnosing breast cancer. Although this does not prevent the disease, diagnosing breast cancer as early as possible can save lives.

In the past, women who came in with a lump were found to have breast cancer. Nowadays, radiologists find cancer via mammography early in the disease development, and often before a patient can feel it. Usually, these earlier stages also have far lower lymph node involvement.
While mammograms do not prevent breast cancer, they have been shown to reduce mortality by 35% in women over 50 years old; in women between 40 and 50, studies have shown that mammograms may lower the chance of dying from breast cancer by 25-35%. By using mammography to detect localised breast cancers at an early stage there is less need for surgical breast removal.
Mammograms are far from perfect: breast tissue can conceal a growing cancer and prevent it from showing up on the mammogram (women with breast implants are additionally prone to this). Many health experts agree that the biggest misconception about mammography is that is picks up every breast cancer. However, this is not the case - mammography actually misses at least 10% of all breast cancers. Women should always practice self-examination and bring any lump they feel to their doctor’s attention to have it evaluated.
However, mammograms remain one of the most important tools to help doctors to diagnose and evaluate women who have had breast caner, and leading experts, the National Cancer Institute, the American Cancer Society, and the American College of Radiology now recommend annual mammograms for women over 40 years old.
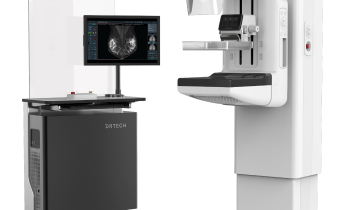
The technique of X-ray imaging has been used for roughly thirty years, with digital technology now being utilised increasingly to improve image quality and increase patient comfort.
A novel digital mammography system manufactured by Siemens, which optimises clinical workflow, has been tested in clinical trials and appears to have all the qualities for becoming the new benchmark in X-ray technology in digital imaging of the breast. Besides offering the latest in digital technology, it provides advantages in patient comfort as well excellent image quality based on amorphous selenium (a-Se). It also offers an optimised solution from screening and diagnosis through biopsy, to evaluation, follow-up and archiving in a single system.
The large format size of the digital plate allows imaging even of large breasts in a single image, permitting the entire breast as well as a larger area of the pectoral muscle to be included. Through a special function, examination is less painful - compression of breast tissues is controlled and optimised to exert only minimal pressure while ensuring optimal digital quality of the entire breast.
A group of clinical researchers led by Schulz-Wendland, Professor of Gynaecological Radiology at the Institute of Diagnostic Radiology, University of Erlangen-Nuremberg, Germany, conducted an experimental investigation - a so-called phantom study using wax blocks - to compare image quality in X-ray mammography. They compared results using conventional screen systems (SFS) with those using this new full-field digital mammography unit (DR) with an amorphous Se-detector, determining the differences in image quality delivered by both systems.
In their investigation, radiograms were acquired by both the conventional film screen system as well as the digital system. A phantom was constructed of wax blocks that could be variably arranged into columns and rows. The thickness was 45 mm in agreement with the standard phantom in the European Protocol on Dosimetry in Mammography. Some blocks contained nylon strings, some contained aluminium oxide grains, and others were empty, whilst still others contained round lesions with blurred margins to simulate the contours and textures of breast tissue.
When primary dosimetry was completed, the results were compared, using both imaging modalities and X-rays. The five investigators noted their observations for every finding of the 16 wax blocks: ‘g’ for grains, ‘l’ for round lesions, ‘s’ for strings and ‘e’ for empty. Results were then compared with the true arrangements, whereby the test for recognition was planned only for true positive results. In other words the sensitivity of the two systems was proved. For each modality a maximum of 45 true positive results were possible (18 strings, 15 grains, 12 round lesions).
The results showed that using conventional film screen system mammography, a total summary of 191 (average 38.2) of 225 possible details were detected by the five investigators, compared with a summary of 219 (average of 43.8) using digital mammography. Based on these experimental findings, the researchers conclude that, from the two modalities, full-field digital mammography shows better results in the capacity for detection of details, despite lower resolution (7 lp/mm vs. 14 lp/mm). The limit due to lower resolution is compensated in this system by higher DQE (detective quantum efficiency) and signal-to-noise ratio.
The researchers conclude that their phantom study shows the possibility for replacing conventional film screening systems with digital mammography (DR) that includes a newly developed a-Se-detector.
With X-ray technology modernising, as in this new Siemens device, screening women with breast cancer enters a new era. The goal is to have mammography as a highly reliable diagnostic tool for breast cancer, with the potential to become a widespread screening device employed routinely, so that the majority of breast cancers can be detected in their incipient stage.
01.07.2004