© Gorodenkoff – stock.adobe.com
News • Unintended effects
Telling women that they have dense breasts may do more harm than good
Leaves some women anxious and confused about their breast health and may increase demand on health services, say researchers
Recommendations introduced in Australia and being considered in the UK to tell women if they have dense breasts as part of their screening results may have unintended effects and increase demand on health services, finds a clinical trial designed to assess the real-world impact of notification, published by The BMJ.
What we found in practice was that breast density notification made women more confused and anxious about their breast health. Women also did not feel more informed
Brooke Nickel
The results show that women who were notified of their dense breasts (which can hide small cancers on a mammogram, making them harder to detect) felt more anxious and confused about their breast health 8 weeks after their screening appointment, and were more likely to want advice from their general practitioner (GP) about what to do next, despite the lack of clear evidence-based and equitable clinical pathways.
Lead author of the new study, Dr Brooke Nickel from the University of Sydney's School of Public Health, said: “Breast density notification is based on the premise that giving women information will empower them to make individual choices about their health. In theory this is a really good thing but what we found in practice was that breast density notification made women more confused and anxious about their breast health. Women also did not feel more informed.”
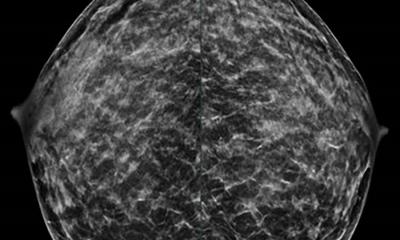
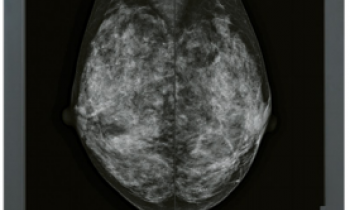
Estimates suggest that between 25% and 40% of women have denser breast tissue which can increase the risk of developing cancer and make it harder for cancers to be detected through a mammogram.
Breast density notification is already mandatory in the US, is moving in that direction in Australia, and being considered in other countries including the UK on the premise that it helps women to make more informed decisions about their breast health. But robust evidence on whether the benefits of notifying women who are having mammography screening outweigh the potential harms is lacking.
To address this knowledge gap, researchers in Australia set out to investigate the real-world impact of notifying women of their dense breasts on their psychosocial outcomes and their health service use intentions. Their findings are based on data from 2,401 women (average age 57) screened as part of the national population-based screening programme between September 2023 and July 2024 who were classified as having dense breasts (BI-RADS category C and D).
Recommended article
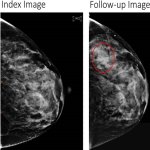
News • Radiomic parenchymal phenotypes
Dense breasts = high cancer risk? It's not that simple
Using radiomics on mammograms of over 30,000 women, researchers have identified six breast texture patterns that may be associated with increased cancer risk.
Details such as age, language/s spoken, and personal and family history of cancer were collected and women were randomised to either standard “control” care (no notification of breast density in their results letter), notification of breast density plus written information about breast density and its implications (intervention 1), or notification of density plus a link to online video based information (intervention 2). After 8 weeks, women reported their prior awareness of breast density, self-rated health and wellbeing, health literacy, and preferences for more or less healthcare. They were also surveyed about their psychological response to their results (feeling anxious, confused, or informed) and their intentions to talk to their GP and pursue additional screening.
Compared with the control group, women notified of their breast density had greater odds of feeling anxious (control: 18%; intervention 1: 20.8%; intervention 2: 20.5%) and were significantly more confused (control: 2.7%; intervention 1: 11.5%; intervention 2: 9%) about what to do. Both notified groups also had significantly higher intentions to talk to their GP about their screening results (intervention 1: 22.8%; intervention 2: 19.4%) compared with the control arm (12.9%), although most women did not intend to have additional screening.
And notified women did not feel better informed to make decisions about their breast health compared with controls.
The authors acknowledge several limitations including the low proportion of women who did not access or watch the additional video-based information in full, as well as the low proportion of women from non-English speaking backgrounds in the trial. However, they say this is the first international trial to rigorously evaluate the immediate consequences of breast density notification, providing key evidence for breast cancer screening programmes outside of the US contemplating introducing density notification or legislation.
Dr Nickel concludes: "Internationally, we encourage governments to consider gathering additional data on beneficial and equitable clinical pathways and to plan the provision of breast density information carefully to ensure that the benefits of breast density notification outweigh potential harms for all women.”
Source: The BMJ / University of Sydney
04.12.2025