Article • Surgery to reduce obesity-related mortality
When diet and excercise alone are not enough
Obesity not only means someone is overweight but, over time, they will probably suffer sequelae that increasingly impair quality of life and are potentially fatal – these include hypertension, coronary heart disease, type two diabetes, pulmonary function disorders, tumours, plus an increased risk during surgery and anaesthesia.
Report: Anja Behringer
In patients with morbid obesity, class three obesity, according to the WHO classification, conservative therapies such as change of diet and physical exercise rarely lead to the desired weight loss and, even more importantly, weight loss is rarely permanent. ‘While bariatric surgery has been considered the last resort for patients with a BMI above 40, it can be first choice, particularly in the presence of severe co-morbidities, since it achieves significant – and permanent – weight loss and can improve or even cure co-morbidities such as type two diabetes,’ says Professor Dr Thomas Rösch, Director of the Clinic and Polyclinic for Interdisciplinary Endoscopy at University Hospital Hamburg-Eppendorf.
Recommended article

News • Place matters
Obesity and the "ecology of disadvantage"
Nearly 70 percent of the U.S. adult population meets the definition of overweight or obese, but a new study by University of Arkansas researchers shows the problem isn’t randomly distributed across the country. Instead, obesity is concentrated in areas with social and demographic factors that create what researchers term an “ecology of disadvantage.”
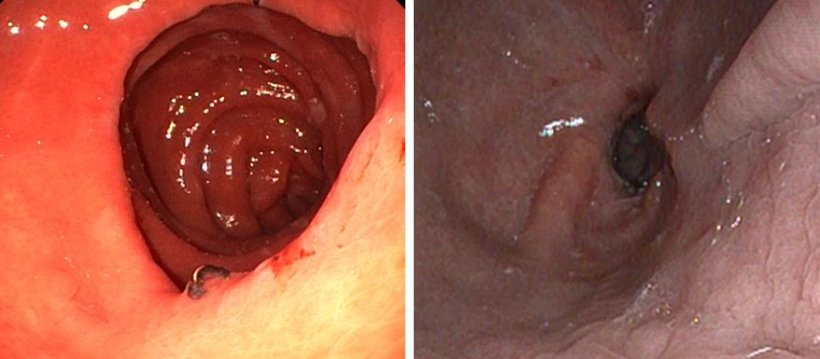
The appropriate surgical procedure depends on the overall status of the individual patient, co-morbidities and dietary behaviour – there is no single gold standard. At Viszeralmedizin 2018, the congress of the German Society of Gastroenterology, held in September, Professor Rösch presented some new endoscopy methods for patients with a BMI of 35 to 45.
The objectives of surgical obesity treatment have changed significantly. When bariatric surgeries were first performed in the 1950s weight loss was the one and only goal. A decade later, gastric bypass surgery was developed, which, since 1994 can be done laparoscopically. Today, the aim is a sustained 50 percent reduction of overweight. In addition, improvement or remission of obesity-related diseases, improved quality of life, prevention of sequelae and reduction of obesity-related mortality are major objectives – not to mention cost savings due to improved health status.
Prior to surgery, every single patient is recommended to undergo indication assessment conducted by an interdisciplinary team in an obesity centre, including patient information on the suitable surgery options.

The German Society for General and Visceral Surgery (Deutsche Gesellschaft für Allgemein- und Viszeralchirurgie - DGAV) has so far certified four excellence centres in Germany. The only university-based obesity centre is located at University Hospital Hamburg-Eppendorf and received the highest of three certification levels.
The DGAV and the International Federation of Surgery of Obesity (I.F.S.O.) demand the following criteria for surgical obesity intervention to be met:
- BMI >40 kg/m²
- BMI >35 kg/m² with severe co-morbidities
- obesity has been present for more than five years
- no metabolic diseases
- no unstable mental disease
- no alcohol and/or drug abuse
In addition, the patient must be able to cooperate and the surgical risk has to be acceptable.
The higher the complexity of the intervention – gastric band, sleeve gastrectomy, gastric bypass – the better the outcomes in terms of blood glucose management and remission rate.
Research has shown that reversible interventions such as a gastric balloon, or gastric pacing, have no long-term benefit. ‘Removal often leads to relapse, that is weight gain,’ says Professor Rösch. ‘Nevertheless, these surgeries are frequently offered on the “grey market”.’
Whilst in the past morbid obesity surgery was performed conventionally, today it is done minimally invasively (i.e. keyhole surgery). Endoscopy, a method without external access, is even less invasive. ‘This less invasive access also means a reduced risk for the patient, and it is less intricate, which translates into cost savings,’ says Professor Rösch. The latter issue is important because statutory health insurers often refuse to pay for bariatric surgery. Very often, patients are not recognised as multi-morbid and surgery is not considered to have a long-term and life-saving effect. In Germany, surgeries, if performed at all, are often performed too late.
However, positive outcomes also depend to a large extent on improved infrastructure: out-patient follow-up plans for obese patients in specialised health centres offering an interdisciplinary and multimodal level scheme. The new endoscopic methods, moreover, still need to prove their long-term efficacy. Nevertheless, it might be useful to integrate them into the treatment portfolio of an obesity centre.
Profile:
Professor Thomas Rösch has directed the Department of Interdisciplinary Endoscopy at University Hospital Hamburg-Eppendorf (UKE) since late 2008. After medical studies at Munich’s Technical University he joined its clinical team. In 2004, now senior physician and Head of Endoscopy at TU’s Medical Clinic II, he was appointed Professor at Charité Berlin’s Gastroenterology Clinic. Up to 2008, he headed the department of interdisciplinary endoscopy department. His clinical focus lies on diagnostics and therapy of Barrett’s oesophagus and early gastrointestinal carcinoma, diagnostic endo-ultrasound and pancreatobiliary interventions using ERCP and endo-ultrasound; he also researches preventive colonoscopy care, along with gastroenterologists in Hamburg and Berlin. Since 2015 his research has increasingly taken place at the new Oesophagus Centre at UKE.
20.11.2019





