Article • New Techniques
‘Very few people have a carbon hyper-polariser’
From the extremely new, but not generally available, to the somewhat new… very available and highly useful… Walter Kucharczyk outlines potentials and practicalities in advanced brain tumour Imaging.
Report: John Brosky
When the organisers of Garmisch MR 2017 (22 January) wanted to hear about the newest developments in neuro radiology, they turned to Walter Kucharczyk MD FRCPC, one of the event’s most experienced presenters, having delivered lectures at this MRI Symposium since 1991.
His experience also includes having served as the President of the International Society of Magnetic Resonance in Medicine (ISMRM), the largest research and education group in the world devoted to developing and teaching magnetic resonance to doctors and scientists, and as previous Professor and Chair of the Department of Medical Imaging at the University of Toronto for sixteenyears. He is a renowned veteran lecturer with a decades-long record of international lectures.
The faculty’s proposed title for the talk was terse, yet ambitious: ‘Brain tumours: what is new?’
Among those attending his presentation, Kucharczyk had predicted that, while many would be interested in and aware of the very newest developments in neuroradiology, most practitioners would not have had access to such equipment and methods, so they would look for advanced, “somewhat-new” techniques that might not be the newest, but are available, are of proven value, and have stood the test of time. ‘For this reason, I divided the lecture into two, between readily available, useful methods, that may not be extremely new, and what is truly new, but not readily available, is also complicated to analyse, and thus not particularly useful to most radiologists today,’ he explained. ‘I hope both parts of the lecture were of interest to the audience – letting them know what all of them can do today and giving them a taste of what might be useful in the near future.’
After setting a context in reviewing the not-so-new, but well-proven techniques, Kucharczyk advanced into more recent developments in techniques that are sufficiently available for everyone to use, and which are useful for a variety of applications, including diffusion weighted imaging, tractography, perfusion MRI, and MR spectroscopy.
The very newest techniques are mostly performed in a research environment to investigate and help solve yet unsolved problems. But, they are not widely practiced because not every medical imaging centre has the hardware, software, cyclotron, combined MRI-PET scanner, carbon hyper-polariser, or specialised personnel to perform these techniques. ‘I don’t think we are there yet with many of the very newest things,’ he pointed out.

The usefulness of the most readily available radiotracer, 18-FDG, to image brain tumours is limited, he said, because radiotracers based on glucose provide poor image contrast between the tumour and normal brain. Brain tumours and healthy brain tissue both avidly take up the glucose. ‘As a result you need to go to other novel formulations of radiotracers, which are very expensive and have very short half lives,’ Kucharczyk explained. ‘These necessitate having a cyclotron.’
Similarly, hyper-polarised carbon species carry similar logistic and cost issues of requiring a very expensive carbon hyper-polariser, he added, ‘but they do enable the radiologist to study carbon-based metabolites, such as pyruvate, through its biochemical pathways and potentially assess the effectiveness of therapeutic drugs. But very few people in the world have a carbon hyper-polariser because it costs something north of a million dollars, and then it has to be placed beside the scanner because the tracers have very short half-life.’
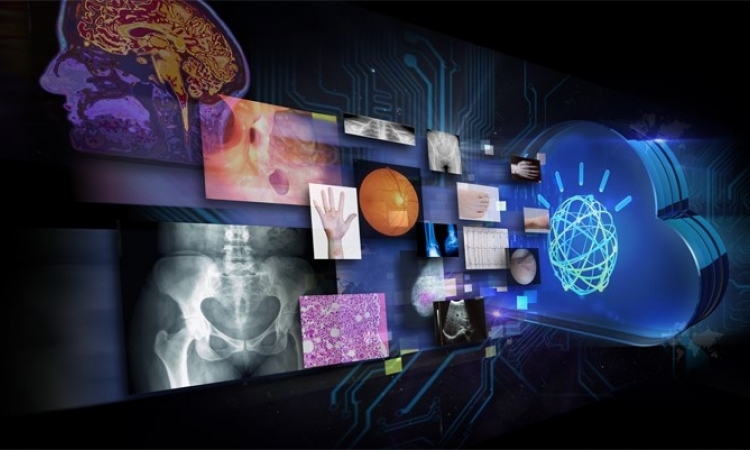
Following the lecture a discussion of developments fell into the category of automated image analysis, big data and machine learning, he said. ‘There is work being done on very interesting concepts based on automated image analysis and machine learning. When we humans look at an image, we see patterns that are based on the spatial location of dots, their Grayscale or colour, and shapes. But digital images can yield additional information already embedded in them, based spatial frequencies and similar features, that can only be extracted by various mathematical operations and transforms, and not appreciated by the human eye,’ he explained.
‘When we analyse this scatter image we can’t say whether it’s a picture of a human brain or a giraffe. But, with appropriate software, a computer can recognise patterns that we cannot, potentially finding unique patterns that may ultimately prove diagnostic of certain diseases. By analysing sufficiently large sets of such image data, perhaps soon automated analysis will enable us to distinguish between various types of brain tumours, grade them, and possibly even inform us of their genetic makeup,
’Looking ahead, Kucharczyk said he hopes that radiologists, like machines, can learn from the detailed correlative analysis of clinical information, images, and pathology studies to deliver findings that increasingly correlate with the ultimate pathology report. ‘As radiologists, we are quite accurate in macroscopic diagnosis. We can see many things about a brain tumour that a pathologist does not: the extent of a tumour, its size, and whether there is more than one tumour. And we can provide a fair estimate of the grade and histopathology of the tumour.
Wouldn’t it be cool if we could actually determine the same findings from the images as the pathologist does from the microscopy?
Walter Kucharczyk
‘Today, the pathologist has the final say in brain tumour diagnosis and, by definition, has the definitive opinion on grade, mitotic rate, histopathology and genetic profile, with terms such as: 1p19q co-deletion to determine the chromosomal type, IDH 1 and 2 mutation [isocitrate dehydrogenase], and the MGMT promoter methylation status,’ he said. ‘These are all important in determining diagnosis, prognosis, and probability of treatment response.
’Then, he speculated: ‘Wouldn’t it be cool if we could actually determine the same findings from the images as the pathologist does from the microscopy?’
Continuing: ‘Ultimately our objective should be to be able to do everything the pathologist does, but to do it in vivo, by extracting that information from images. Our objectives should be to determine all features of the diagnosis and prognosis without having to operate on the patient, without having to extract tissue. Are we there yet? No way. Will we ever get there? Probably not completely, but we are moving in that direction,’ Kucharczyk concluded.
Profile:
Walter Kucharczyk, MD, FRCPC is the Director for Research at the Joint Department of Medical Imaging of the University of Toronto and a hands-on Neuroradiologist there, as well as a Professor of Medical Imaging and Neurosurgery.
03.03.2017