News • Targeted drug activation
Ultrasound-triggered chemotherapy to reduce side-effects
Chemotherapy has long been a cornerstone of cancer treatment, but its effectiveness comes at a cost.

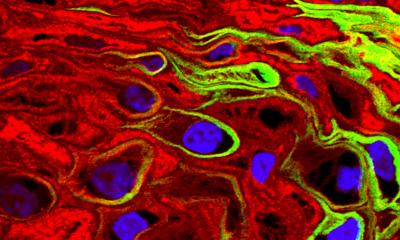
Image source: Syracuse University
The powerful drugs used to kill cancer cells often damage healthy tissues as well, leading to side effects ranging from nausea and fatigue to organ damage. At Syracuse University’s College of Arts and Sciences (A&S) and BioInspired Institute, a team of researchers is working to change that.
Xiaoran Hu, assistant professor of chemistry in A&S, has developed a method that could allow cancer-fighting drugs to be triggered precisely where they’re needed—inside tumors—while sparing the rest of the body. Hu and his team, which includes researchers from the Department of Chemistry, recently published their findings in the journal Chemical Science. Their paper explores how ultrasound waves can be used to activate chemotherapy drugs only in targeted areas, offering a new path toward safer, more effective cancer treatment.
“As an initial step toward developing a generally applicable platform, this approach holds promise for spatially controlled release of cytotoxic drugs in ultrasound-irradiated tissue regions, minimizing off-target side effects. To put it simply, if a handheld ultrasound instrument or tool at the bedside can be used to guide or activate drugs, many patients could benefit in the future,” says Hu.
At the heart of their research is the concept of a prodrug—a compound that remains inactive until it’s triggered to unmask its therapeutic effects. Traditionally, prodrugs are activated by internal conditions like low pH or specific enzymes found in tumors. However, these triggers can also be present in healthy tissues, leading to unintended side effects.
Hu’s team is taking a different approach. Instead of relying on internal triggers, they’re using ultrasound, a safe and non-invasive technology commonly used in medical imaging. Unlike light-based activation methods, which struggle to penetrate deep tissues, ultrasound can reach tumors located deep within the body and be precisely targeted.
Recommended article

Article • Focus on treatment and research news
Chemotherapy: effective against cancer, at a cost
Chemotherapy is used against various cancers and is often consideres as a last resort – especially if the cancer has metastasised. Since chemotherapy agents can cause severe side effects, research aims to make treatment more tolerable. Keep up-to-date with the latest research news, medical applications, and background information.
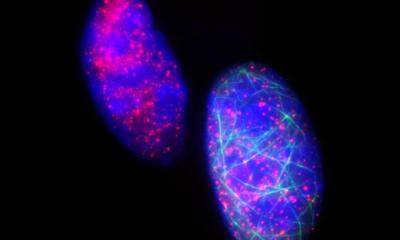
The process begins with a specially designed prodrug that remains inactive as it circulates through the body. When ultrasound is applied to a specific area—such as a tumor site—it generates hydroxyl radicals, short-lived reactive species that trigger a chemical transformation in the prodrug. This transformation releases the active drug precisely where it’s needed, restoring its cancer-fighting power while minimizing toxicity to healthy cells. “Ultrasound is a widely used imaging technology, but its chemical effects remain largely unexplored in biomedical contexts. Our team aims to harness ultrasound to drive beneficial chemical reactions in biology and medicine. The strategy in our newest publication allows for externally controlled release of drugs in ultrasound-irradiated regions,” says Hu. “It holds promise to minimize side effects while enhancing treatment precision.”
The implications for cancer care could be significant. Oncologists could use existing ultrasound equipment not only for diagnosis but also to activate chemotherapy drugs during treatment. This dual use could streamline care and improve outcomes. “Ultrasound is already integral to oncology procedures, such as breast cancer diagnosis and interventions,” Hu notes. “Our platform leverages this trajectory and is potentially translatable with existing ultrasound infrastructure.”
While the technology is still in its early stages, Hu and his team are optimistic about its future. They’re now working to refine how the ultrasound activates the drugs, making the release process even more efficient. They're also collaborating with other researchers to move this technology closer to potential use in patients.
Another key aspect of this project is the valuable training it has provided. Xuancheng Fu, a postdoctoral scholar in Hu’s lab, helped lead the project from material synthesis to chemical characterization and cell-based experiments. Graduate students Bowen Xu, Hirusha Liyanage and others contributed by optimizing experimental conditions and collecting data. Undergraduate research assistants, including Luke Westbrook, Seth Brown and Tatum DeMarco also gained valuable research experience through this project. “This kind of hands-on experience is invaluable,” says Hu. “It prepares students to tackle real-world challenges and contribute meaningfully to the future of medicine.”
The potential impact of Hu’s research extends far beyond the lab. By enabling more precise drug delivery, the technology could one day reduce the physical and emotional toll of chemotherapy, improve patient outcomes and lower healthcare costs.
As the team continues to refine their method and move toward animal testing, their work exemplifies the kind of innovative, interdisciplinary research happening at A&S—research that not only pushes the boundaries of science but also holds the promise of improving lives.
Source: Syracuse University
07.11.2025