Turf wars
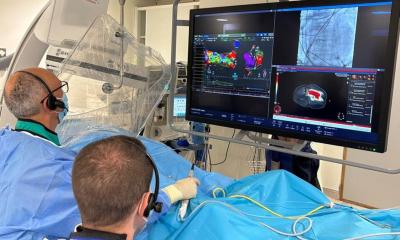
Nowadays, no radiology conference would be complete without a discussion on turf battles. The rapid development and broad acceptance of cardiac CT has exceeded expectations, and both radiologists and cardiologists are incorporating this technology into their practices. Educational courses on cardiac CT are in high demand and well attended by both radiologists and cardiologists.

University of California Los Angeles
(UCLA, USA)
Radiologists typically harbour a number of resentments when they see the increasing number of cardiologists moving into the cardiovascular CT field. They generally believe that technical understanding and sophistication should be the defining attribute when defining who should control imaging technology, and rely on the comprehensible perception that cardiologists may lack knowledge about CT technique and equipment, radiation physics and safety. Radiologists are often frustrated that other medical professionals frequently do not share this perspective. Many radiologists view cardiologists as the group of physicians that has already taken from them coronary angiography, echocardiography and increasingly renal and peripheral artery interventions. They perceive the cardiologist’s interest in cardiac CT as just another example of infiltrating their turf.
On the other hand, cardiologists feel that they have more expertise in invasive coronary angiography, better understanding of cardiac anatomy and pathology and better understanding of the clinical implications of normal or abnormal findings of a cardiac CT study, so they can find the best way to integrate results with patient management. They feel that cardiovascular CT – under their control – will help them to better control their patients and that they should be the logical heirs of this modality.
In addition they often regard CT imaging as a mandatory tool to increase revenues in a declining reimbursement environment. However, depending on the political environment of medical practice, governmental action has increasingly been noticed in regulating who can own and operate imaging equipment in order to avoid the practice of unlimited self-referral.
A detached view of turf issues allows a less emotional assessment. Although turf issues may be initiated by technologic innovation, they are basically not about technology alone, but rather about how the technology can be implemented in an existing business or medical practice model. As a general concept, technology by itself has limited value until it finds a place in a business model or, in other words, until someone is willing to pay for it. Since the radiology practice model relies so heavily on technology, both radiologists and cardiologists need to understand the interaction of a new technology with a medical practice model, a relationship that is not always intuitive. CT is an example of a new technology that has revolutionised radiology. The main reason for the successful implementation of CT was that radiology could integrate CT into its business model without major difficulty. Interestingly, CT was initially marketed to neurosurgeons. However, CT failed to find a home in their business model since neurosurgery could not incorporate this high-cost technology, compared with radiology with its generally large-scale imaging operation and wide base of referring physicians. Consequently the successful adoption of CT enabled the integration of MR imaging without major problems.
Cardiologists commonly control a large number of patients with potentially significant amounts of yet undiagnosed cardiovascular disease. CT as a non-invasive modality can be utilised to examine these patients. Cardiologists might be tempted to employ a variety of treatment strategies when they find even asymptomatic disease in various vascular areas. Whether, due to potentially unnecessary therapeutic measures, such an approach raises overall healthcare costs, or if early diagnosis and treatment might prevent disease and therefore save costs, remains controversial. Since radiologists usually depend on referrals, they are less susceptible to self-referral issues. Given that radiologists generally have imaging expertise that cardiologists lack, e.g. better knowledge of peripheral vascular anatomy or nonvascular pathology in the chest, it appears justified that radiologists are required to also read all CT studies for potential nonvascular findings.
On the basis of this analysis, it should be clear that a simple duplication of a practice model for cardiac CT to be operated separately by cardiologists and radiologists offers no real competitive advantage for either side. A joint model, based on true teamwork, with the idea of division of labour and responsibilities, could yield a mutually successful strategy. Both physicians and patients might benefit from an interdisciplinary approach that utilises both cardiologists and radiologists to make treatment decisions.
08.03.2007