Peripheral artery disease
Treating poor blood circulation with injectable gel
Bioengineers and physicians at the University of California, San Diego have developed a potential new therapy for critical limb ischemia, a condition that causes extremely poor circulation in the limbs and leads to an estimated 230,000 amputations every year in North America and Europe alone to prevent the spread of infection and tissue death. The new therapy could prevent or limit amputations for a condition that affects more than 27 million people and is a manifestation of advanced peripheral arterial disease.
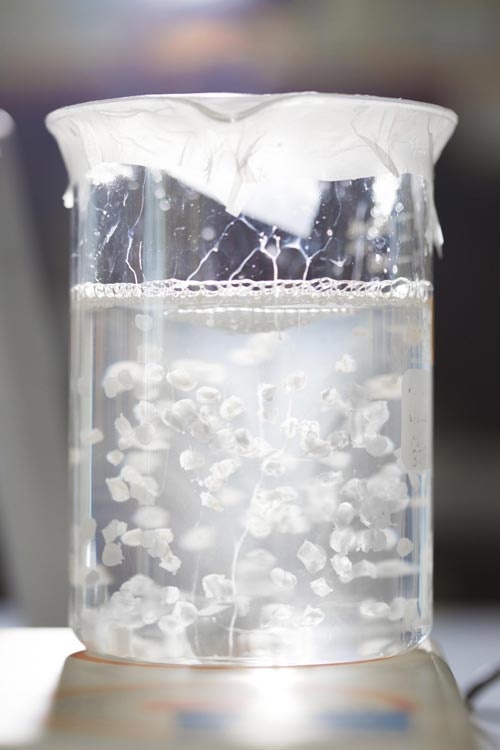
The therapy consists of injecting in the affected area a gel derived from the natural scaffolding, or extracellular matrix, in skeletal muscle tissue. The team tested the procedure in a rat model of the disease and found that it promotes muscle remodeling and improves blood flow. They published their findings recently in the inaugural issue of the Journal of the American College of Cardiology: Basic to Translational Science.
"This is a unique approach that not only helps repair the damaged vascular system, but also helps restore muscle tissue," said Karen Christman, a professor of bioengineering at the Jacobs School of Engineering and the Sanford Consortium for Regenerative Medicine at UC San Diego and the paper's senior author.
"Avoiding or limiting extent of amputations is a huge benefit for patients," said Dr. Ehtisham Mahmud, chief of cardiovascular medicine at the Sulpizio Cardiovascular Center at UC San Diego and a study co-investigator.
Christman and Mahmud partnered to make sure the study's design would eventually help patients when the therapy was ready for the clinic--a step that should take about two years. "This is what makes UC San Diego unique," said Mahmud. "We are bringing together engineering and medicine and demonstrating the translational implications of preclinical research."
As far as researchers know, no one had tried to use an injectable material by itself to treat both the low blood flow and weakened skeletal muscle in critical limb ischemia.
Peripheral arterial disease and critical limb ischemia
Peripheral arterial disease patients suffer from poor circulation in their limbs, which can lead to critical tissue damage. The condition is associated with atherosclerosis in old age, diabetes and smoking. It affects men and women equally. In the most extreme form, called critical limb ischemia, a severe obstruction of arteries in the limbs reduces blood flow to hands, feet and legs. Some of Mahmud's patients experience severe pain in their limbs. Some already suffer from tissue necrosis, or amputations. Others suffer from wounds that won't heal and get infected because they lack proper blood supply.
For these patients, traditional surgery or endovascular procedures can often reestablish normal blood flow. But when these interventions fail or aren't possible, limited options remain. So far, potential therapies for these patients, including using growth factor, gene or cell therapy, have proven problematic and costly. Amputations end up being a common option for treatment in severe cases of critical limb ischemia, Mahmud said.
Injectable gel therapy
Christman's team had already shown that injection of a gel derived from cardiac muscle tissue extracted from pigs could help repair the heart after a heart attack. The tissue is stripped of cells, leaving behind a scaffold of the extracellular matrix from cardiac muscle, which acts a regenerative environment where cells can grow again.
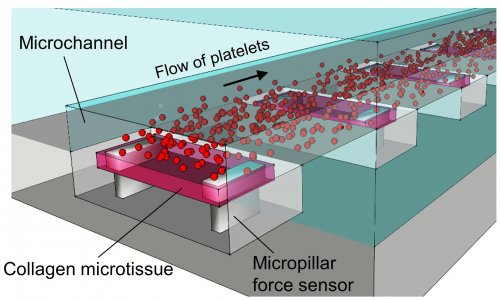
Using this same concept, Christman and her team now are turning their attention to peripheral artery disease and critical limb ischemia. They developed a material that was derived from the skeletal muscle of pigs to treat damaged skeletal muscle in these patients. Researchers injected the gel into the affected area in a rat model of the disease seven days post-surgery and monitored blood flow in the rats' limbs up to 35 days after injection.
Researchers found that the hydrogel increased the diameter of the rats' larger blood vessels, called arterioles. The increased diameter led to improved blood flow in the limbs. By day 35, the size and structure of muscle fibers in the rats treated with the hydrogel was comparable to that in healthy rats.
The gel, which forms a fibrous scaffold upon injection, also attracted muscle stem cells to the affected area. Gene expression analysis showed that inflammatory response and cell death decreased while blood vessel and muscle development pathways increased in rats injected with the gel.
Next steps include looking at other disease models in animals and refining preclinical safety protocols and quality control for manufacturing. Ventrix, a startup cofounded by Christman, partially licensed the technology from UC San Diego for clinical applications.
Source: University of California, San Diego
15.03.2016