The importance of MRI for gynaecological malignancies
Hedvig Hricak, Chair of the Radiology Department at the Memorial Sloan-Kettering Cancer Center, New York, USA, describes emerging applications and potential trends in gynaecological cancer treatment described at the 15th International Symposium Crossing Barriers

Combining technological advances, new clinical management paradigms and discoveries from epidemiology and biology has been and remains the hallmark of our specialty. The presentations at the 15th International Symposium, Crossing Barriers, are in keeping with this tradition and show how our profession continues to elevate the quality of clinical care by applying increasingly powerful imaging techniques to clinically relevant questions. MRI has become integral to the diagnosis and management of patients with gynaecological malignancies, as it provides exquisite anatomical detail and allows quantitative, multiparametric functional assessment of tumours. Adding functional sequences – such as dynamic contrast-enhanced MRI (DCE-MRI), diffusion-weighted MRI (DW-MRI) and most recently Intravoxel incoherent motion (IVIM) MR imaging – to conventional MRI, has been found to be particularly helpful for lesion characterisation, assessment of tumour response to treatment and differentiating post-treatment changes from tumour recurrence.
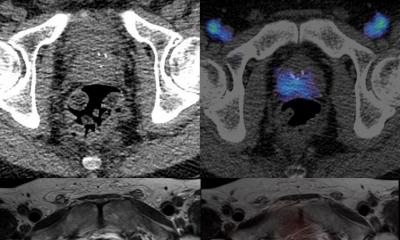
The emerging hybrid imaging modality PET/MR has the capacity to combine anatomical detail with an even richer supply of functional and metabolic information and will fundamentally change the way we evaluate gynaecological cancer patients. Its application in the laboratory as well as the clinic will aid drug discovery and enable the delivery of substantially more individualised cancer care. The value of PET/MR will be further enhanced by the advent of clinical hyperpolarised MRSI (HP-MRSI). Clinical HP-MRSI can increase the MR signal 10,000–100,000-fold, allowing imaging of nuclei other than 1H with unprecedented sensitivity and speed. Thus, it not only can identify the location and quantity of a targeted hyperpolarised agent, but can also identify the agent’s downstream enzymatic products, elucidating an entire chain of metabolic events in vivo.
Multiple hyperpolarised substances can be injected and examined simultaneously, enabling multiple metabolic pathways to be probed in the same imaging session. With clinical HP-MRSI, imaging is crossing a threshold into a new level of real-time, quantitative assessment of tumour biology that will open up unprecedented opportunities for developing powerful predictive, prognostic and early response biomarkers for cancer management. HP-MRSI, conventional MRI, and PET have different, yet complementary strengths. In the future, combined PET/MR/HP-MRSI will allow results from the various imaging approaches to be precisely correlated – providing new insights into cancer biology and increasing the value of imaging biomarkers in both drug development and clinical care.
MRI’s role in gynaecological oncology
MRI has become integral to the diagnosis and management of patients with gynaecological malignancies as it combines exquisite anatomical detail with functional, multiparametric and quantitative assessment of tumour burden and its response to treatment. Techniques such as dynamic contrast-enhanced MRI (DCE-MRI) and diffusion-weighted MRI (DW-MRI) enable the radiologist to move from morphological to functional assessment of gynaecological malignancies. In patients with endometrial cancer, MRI plays an important role in pre-operative evaluation and surgical planning: Not only does it allow non-invasive assessment of important prognostic factors such as depth of myometrial invasion, cervical stroma invasion, presence of peritoneal implants and lymphadenopathy, but through the use of functional imaging techniques, such as DW-MRI and DCE-MRI, it can also provide insights into tumour aggressiveness and micro-environment.
In patients with cervical cancer, MRI is the preferred imaging modality for evaluating primary disease, as it can determine tumour location (exophytic or endocervical) and size as well as invasion of the parametria, pelvic side-wall or adjacent organs, and lymph nodes with greater accuracy than clinical examination. Additionally, quantitative DCE-MRI and DW-MRI parameters serve as predictive biomarkers of response to chemo-radiotherapy, thus allowing for individualised tailoring of patients’ treatment. In patients with ovarian cancer, MRI is a problem-solving modality. There is growing evidence that DW-MRI allows more accurate mapping of the extent of peritoneal disease than does CT. MRI plays an important role in patients with recurrent ovarian cancer by assessing the resectability of solitary pelvic recurrences. MRI can help to plan and tailor the pelvic exenterative procedure by accurately depicting local tumour extent and invasion of adjacent organs in patients with treatmentresistant or recurrent gynaecological cancer.
The gold standard
CT is still the gold standard for evaluating disease extent in patients with ovarian cancer, whereas PET/ CT is routinely used to evaluate distant metastatic disease (including lymph nodes) in patients with primary and recurrent gynaecological malignancies. The maximum standardised uptake value (SUVmax) – a quantitative parameter derived from PET/CT – serves as a prognostic biomarker in patients with primary cervical cancer as well as in patients with recurrent ovarian cancer.
MRI’s role in chemoradiotherapy planning and monitoring
MRI plays a central role in planning chemo-radiotherapy and monitoring the response to such therapy in patients with advanced cervical cancer. DCE-MRI parameters reflecting heterogeneous tumour perfusion and subtle tumour volume changes early during chemo-radiotherapy are independent and better predictors of tumour recurrence and poor survival than are clinical prognostic factors. Preliminary data also demonstrate that the apparent diffusion coefficient (a parameter derived from DW-MRI) may serve as a predictive biomarker and has the potential to allow early assessment of response to chemo-radiotherapy.
The benefit of a higher magnetic field
MRI is the most sensitive technique for delineating small lesions due to its superb soft tissue resolution. A higher magnetic field strength improves image quality (due to an increased signal to noise ratio) and enables more effective use of functional techniques such as DW-MRI and DCE-MRI as well as more detailed metabolic imaging with MR spectroscopy.
Will PET/MR give additional clinical information?
This is a very new and exciting area of clinical research. The preliminary reports suggest that PET/MR may provide additional information for tumour staging and thus may influence patient management. In the future, with the development of new, targeted radiotracers, PET/MR will supply powerful biomarkers for multiple purposes.
Future roles
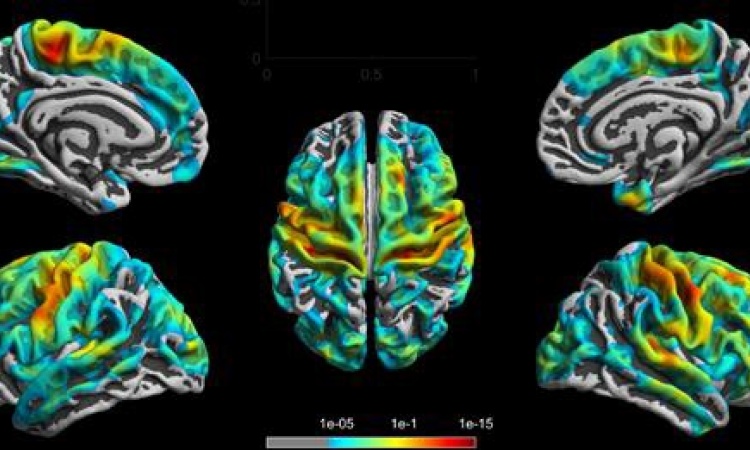
PET/MR, which has the capacity to capture an unprecedented diversity of functional and metabolic parameters in the context of exquisite anatomical detail, will change the way we evaluate gynaecological cancer patients and will greatly aid in drug discovery and the delivery of individualised clinical care. Radiogenomics will provide the ability to match MR imaging traits with genomic information, furthering the development of prognostic and predictive imaging biomarkers. Imaging (by MRI and or PET/MR) will be central to the way we design future clinical trials, as a more adaptive trial design is urgently needed. The use of molecular imaging techniques, including HP-MRSI, will allow the development of more powerful predictive biomarkers, particularly for treatment selection and response assessment. Intraoperative molecular imaging will likely facilitate more complete tumour resection. The development of sensitive molecular imaging biomarkers for ovarian cancer may enable repeat molecular imaging to substitute for preventative oophorectomy in highrisk patients by allowing detection of the disease before symptoms arise.
PROFILE
Born in Zagreb, in former Yugoslavia, Professor hedvig hricak MD PhD Dr (hc) studied medicine at the University of Zagreb and in the Karolinska Institute in Sweden. Today, she chairs the Department of Radiology in New York’s Memorial Sloan-Kettering Cancer Center, and is professor of radiology at Cornell University Medical College and radiologist at Memorial Hospital in New York. In 2010, she presided over the RSNA, and her professional awards include the Marie Curie prize from the Society of Women in Radiology and the Beclere-Medal from the International Society of Radiology. Prof. Hricak’s clinical activities include diagnostic radiology and oncological imaging of urogenital tracts.
10.03.2013