The hidden epidemic: women's cancer in emerging countries
Breast and cervical cancer together account for more than one quarter of all female cancer deaths worldwide, with the majority – including more than 85 % of all cervical cancer deaths – occurring in developing countries. However, a small number of highly effective programs demonstrate that much can be done to reduce risk and increase sustainable access to diagnosis and treatment for these high-mortality cancers in low-resource settings.

In September 2009, The Informal Working Group on Cancer Treatment in Developing Countries (CanTreat International), a coalitation of experts from leading global cancer organizations, released the report "The Hidden Epidemic: Women's Cancers in Low- and Middle-Income Countries". CanTreat International develops new models for the delivery of treatment and palliative care for cancer, particular women's cancer, in developing countries.
Breast and cervical cancer
Early detection is the single most important factor in surviving cancer. For many reasons, however, around 80% of cancer patients in poor countries are not seen by the health services until their disease is advanced, difficult and costly to treat.
Screening a woman for cervical cancer only once between the ages of 35 and 40 reduces her lifetime risk by 25-35%. Currently, only around 19% of women in the developing world are covered by cervical screening, compared with 63% in developed countries.
Where laboratory facilities and expertise for Pap smears are not available, screening can be carried out effectively and inexpensively by visual inspection of the cervix, using staining with acetic acid (vinegar) or Lugol iodine to identify abnormal cells. Such screening can be performed by nurses, even in the most basic primary health care settings.
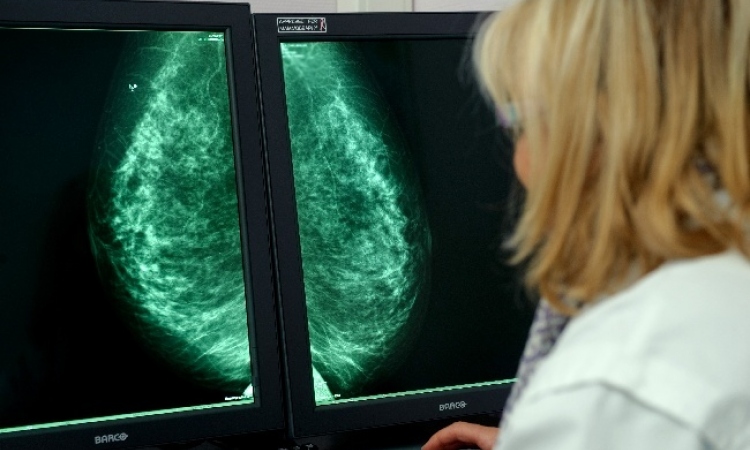
Mass screening for breast cancer with mammography is not feasible in resource-poor settings, but evidence suggests that clinical examination of the breasts by a nurse can be equally effective as a screening method, and is applicalbe even in remote clinics and health centers.
Cancer screening is only effective and ethical if it is part of a well-organized system of follow-up and treatment. In low-resource settings, small precancerous lesions in the cervix can be treated at primary health care level using cryotherapy, a simple procedure that destroys tissue by freezing. Another relatively simple procedure for treating early disease is loop electrosurgical excision (LEEP), which uses a thin wire heated with electricity to remove abnormal cells.
Radiotherapy plays a major role in treatment protocols for both breast and cervical cancer. However, more than 30 countries in Africa and Asia have no radiotherapy services at all.
Late-stage treatment and palliative care
Almost no literature existes on the issue of treatment for late-stage cancer in resource-poor settings. The reality for most women with advanced cancers is that they are sent home to face excruciatingly painful deaths with little or no treatment or care.
Palliative care services for people with untreatable disease are especially important in the poorer regions of the world, where 80 % of cancer patietns present with advanced disease. Yet palliative care is rarely mentioned in national cancer control programs. Access to morphine - the mainstay of cancer pain control and a basic human right according to the World Health Organization - is virtually non-existant in 150 of WHO's 193 member states.
Recommendation for action
Myths, misconceptions and prejudices about cancer are widespread. A crucial first step in addressing women’s cancers is public education designed to reduce stigma and misinformation, as well as to promote changes in women’s behavior to minimize risk and to encourage them to seek timely treatment for any symptoms.
Further challenges to be overcome in addressing women’s cancers in low- and middle-income countries include:
- Lack of awareness and knowledge about cancer among health workers
- Lack of surveillance and statistical data as a basis for planning
- Poor health infrastructure – and the concentration of scarce services in urban areas
- Shortages of skilled personnel, and high costs of drugs and diagnostics
- Inadequate and inappropriate health care systems, geared to dealing with short-term infections rather than long-term chronic diseases
12.01.2010