Article • Immunotherapy
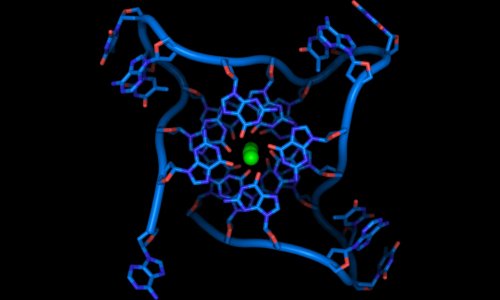
The DNA mismatch repair mechanism
A new genetic study by UK-based scientists suggests that immunotherapy drugs could prove to be an effective treatment for some breast cancer patients.
Report: Mark Nicholls
Scientists from the Wellcome Trust Sanger Institute, near Cambridge – one of the world’s leading genome centres – and their collaborators, have identified particular genetic changes in a DNA repair mechanism in breast cancer. Led by Dr Serena Nik-Zainal, the researchers suggest it could open up the possibility of another therapy option for around 1,000 UK breast cancer patients who could benefit from existing drugs. The study found that a particular group of breast cancer patients have genetic changes, or mutations, that occur due to an abnormality of a DNA repair mechanism known as mismatch repair, which is a mechanism to recognise and remedy mistakes in the genetic code that arise during DNA replication and recombination. The mechanism also repairs some forms of DNA damage.

When cells lack the mismatch repair pathway, mutations build up, which results in cancerous tumours formation. These mutations are found in other cancers, such as colorectal cancer, but are rarely looked for in breast cancer.
In recent work in the USA, colorectal cancers with deficient mismatch repair have been treated with immunotherapies, which exploit the fact that, under the influence of these so-called check point inhibitors, highly mutated tumour cells can be recognised as ‘foreign’ by the patient’s immune system. The results of this new Sanger Institute study suggest that these immunotherapies could also be effective for some breast cancer patients, based on the same mutation patterns seen in their tumours. ‘We’ve unequivocally found mismatch repair deficient breast cancers,’ Serena Nik-Zainal said ‘As these tumours have the same mutational signatures as those of other cancers, like colorectal cancer, in theory they should respond to the same immunotherapy drugs. Our results suggest expanding the cohort of cancer patients that could possibly be treated with checkpoint inhibitors to include these mismatch repair deficient breast cancer patients.’
The study researchers analysed the whole genome sequences of 640 breast cancer tumours and looked for patterns in the mutations, known as mutational signatures, which indicated abnormalities in the mismatch repair mechanism. From the mutational signatures, the team identified 11 tumours that had the mismatch repair defects causing the breast cancer. ‘Using whole genome sequencing we can start to stratify breast cancer patients into different categories based on their mutational signatures,’ said one of the researchers Dr Helen Davies, from the Wellcome Trust Sanger Institute. Current clinical criteria means these tumours would not have been detected as being deficient in the mismatch repair pathway. We have shown that there is, in fact, another category of breast cancers – those with defective mismatch repair.’
Professor Karen Vousden, chief scientist at Cancer Research UK (CRUK), added: ‘Immunotherapies have shown promise for some cancer patients, but the challenge for doctors has been predicting which patients they are likely to help. This study reveals more about the genetic patterns that could show which women with breast cancer are more likely to respond to immunotherapy treatments.’ The next step is to stage clinical trials to determine if immunotherapies could help selected breast cancer patients.
The Wellcome, CRUK, Dana-Farber/Harvard Cancer Centre SPORE in Breast Cancer, and National Research Foundation of Korea with grants from the Korean government, supported this research project.
Profile:
Serena Nik-Zainal MD is a Career Development Fellow (CDF) Group Leader in the Cancer Genome Project at the Sanger Institute in Cambridge and an Honorary Consultant in Clinical Genetics at nearby Addenbrookes Hospital, UK. Having qualified in medicine from the University of Cambridge in 2000, trained as a physician and subsequently specialised in Clinical Genetics, she undertook a PhD at the Wellcome Trust Sanger Institute in 2009. Her research focuses on pursuing biological understanding of the mutational signatures that have been identified in primary human cancers, with a specific interest in breast cancer.
08.02.2018