Article • EUSOBI 2016 Annual Scientific Meeting breast imaging session
‘The best way to screen’
The European Society of Breast Imaging (ESOBI) promotes high quality breast imaging across Europe by developing education and training, encouraging research and promoting guidelines and standards. This year’s meeting (23-24 September) was held in collaboration with the French Society La Société d’Imagerie de la Femme (SIFEM) and drew around 600 radiologists. The event included a two-day course on breast magnetic resonance imaging (MRI).
Report: Jane MacDougall
Aiming to balance the latest in cutting-edge science with everyday clinical practice, this year’s ESOBI meeting featured a session entitled the ‘The best way to screen’. A timely debate in light of the new draft proposal for European guidelines for breast cancer screening and diagnosis that is open for feedback and also when ESOBI are promoting their latest publication ‘Statement in favour of breast screening’.
Nationwide screening programmes result in substantial mortality reductions
Screening with mammography alone is a cost-effective way to save lives. Throughout Europe a substantial reduction in mortality from breast cancer can be seen in those countries that have implemented nationwide screening programmes. Interestingly, the shift from analogue to digital between 2005 and 2010 led to improved results and showed that more high-risk tumours are now detected by mammography.
Of course, there remain drawbacks with mammography screening, such as false positives and over diagnosis. However, so far no other modality has proven to save lives and no information is available regarding the aggressiveness of tumours detected by other modalities, for example the positive predictive value of ultrasound is substantially lower and quality control (operator dependent) is difficult.
For these reasons screening with mammography alone is still the gold standard for population-based screening programmes.
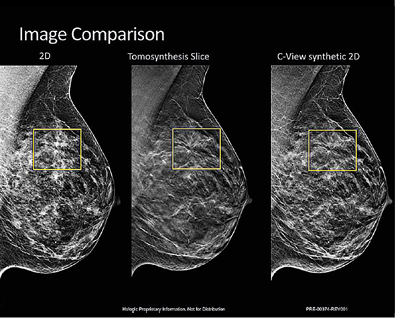
Nevertheless, even screening with full-field digital mammography (FFDM) fails to detect 15-30% of cancers and in women with dense breasts, approximately 7% of the 50-70-year-old population, sensitivity for 2-D mammography can be as low as 58%.
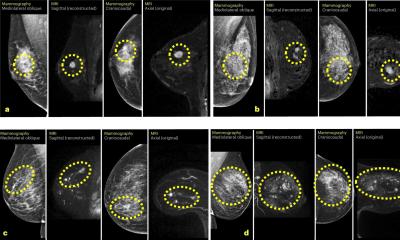
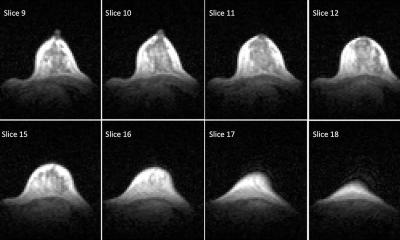
Digital Breast Tomosynthesis (DBT), a 3-D digital mammography system, is a promising tool for improving screening in these women. After X-ray acquisition of a series of 2-D images (projections), reconstruction of the breast is done at different heights above the detector. Current DBT systems are commercialised by five different manufacturers and are routinely used in radiology centres and in several countries, the technique has approval for screening and diagnostics.
Comparison of DBT with FFDM favours DBT
DBT has the potential to improve cancer detection rates with only a small increase in radiation dose. Retrospective reading studies comparing DBT with FFDM have shown improvement in both sensitivity and specificity with DBT. Diagnostic accuracy appears to be largely independent of breast density although benefit appears greater in women with denser breasts. Results are less clear regarding the detection of microcalcification and most studies have found little improvement over 2-D mammography in the detection of ductal carcinoma in situ (DCIS).
Used together in prospective screening studies, DBT with FFDM has demonstrated increased rates in cancer detection compared with FFDM alone. A reduction in false-positive recall rates has also been shown in nearly all studies.
Several DBT issues must now be resolved
Screening with the addition of DBT would approximately double the radiation dose received; but a simulated FFDM image can be generated from a DBT scan. The combination of simulated FFDM images and DBT is being evaluated within several studies and some positive results have been published.
However, before this becomes a realistic proposition for widespread screening programmes several issues around DBT need to be resolved, not least the wide range of totally different characteristics in the machines (angular range, scanning angle, filter/target combination, tube motion, etc.), and the use of different reconstruction methods: filtered back projection or iterative reconstruction.
Also, the additional reading time, the large IT storage, connectivity problems and over diagnosis of low grade cancers will all need to be correctly modelled to obtain cost-effectiveness similar to that of current screening if the addition of DBT is to become a way to improve breast cancer screening.
04.08.2017