© Penn Medicine
Article • ICU response to the Covid-19 surge
Tele-delivery of respiratory therapy services: a resounding success
In their pursuit of solutions for pandemic challenges, a US hospital system applied telemedicine principles to respiratory therapy – with impressive results.
Report: Cynthia E. Keen
When the coronavirus SARS-CoV-2 struck with a vengeance in March 2020, Penn Medicine, a multi-hospital system in greater metropolitan Philadelphia, faced an acute shortage of respiratory therapists (RTs) to treat an escalating number of critically ill patients in respiratory distress. A high demand for RT staff already existed at Penn, which would be exacerbated by the need to remove RTs with underlying medical conditions from the risk of contracting the virus from inpatient bedside work shifts. Hospital management anticipated possible losses among the staff secondary to Covid-19 as well. Finally, various options were considered for limiting exposure and cross-contamination between staff and patients during pandemic-focused and routine care.
To avert this escalating crisis, the hospital system launched a telemedicine respiratory therapist (eRT) service in April 2020, integrating it into the University of Pennsylvania Health System (UPHS) tele-ICU program. First established in November 2004, the Penn E-lert service is a state-of-the-art electronic intensive care unit (ICU) that continuously monitors and evaluates critically ill patients in all UPHS hospital ICUs, proactively identifies impending or evolving patient problems, and assists in or directs on-site clinical management. It is staffed 24/7 by experienced critical care nurses and intensivist physicians from the Departments of Anesthesiology and Critical Care, Emergency Medicine, Internal Medicine and Surgery.
Close to the patient, watching from afar
Initially, the eRT service was staffed at start-up by seven registered RTs with 11 to 24 years of practice, all of whom had health conditions that would not allow them to perform inpatient bedside services due to their high risk of contracting Covid-19. After a limited hours trial during the first 30 days of operation, coverage of the adult ICUs across five hospitals expanded to 24/7 as of May 2020. The service was set up parallel to the existing tele-ICU services and provided coverage for 16 different Covid-19 specific and non-Covid ICUs, with a nominal bed capacity of 320. On-site ICU coverage was maintained at one RT for every 12 patients.
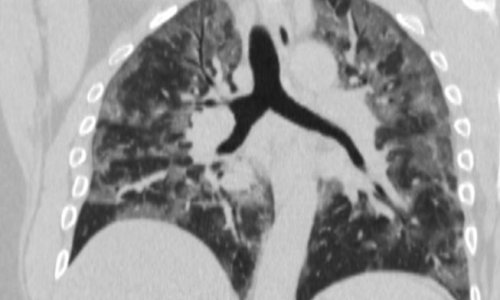
The remote RTs visually monitored both intubated and non-intubated patients experiencing respiratory compromise via ICU-installed cameras, microphones, and specialized systems to deliver tele-critical care services. They completed compliance-required medical documentation, conducted regular ventilator checks, assessed compliance with low tidal volume ventilation, and surveyed endotracheal tube occlusion and reintubations. They also often served as safety officers during high-risk pre-extubation procedures, subsequently remotely monitoring these patients.
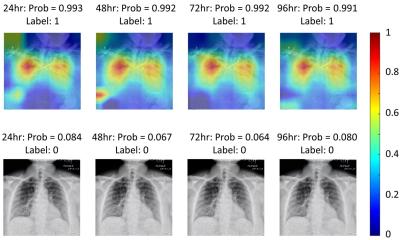
Requests for specialized eRT services could be made by staff in the ICUs in addition to ongoing performed workflow by eRT. The system included an automated alert triggered by the patient’s electronic medical record or an electronic “sniffer” aimed at detecting acute respiratory distress syndrome (ARDS). Clinical staff could also request aid by pushing an emergency button in the ICU and talk to the remote RT immediately by phone.
Much of the immediate acceptance of the tele-RT service is attributed to the protocol that on-site RTs are always in charge of patients. The eRT is a consultative service, and all eRT clinical interventions are carried out only after discussion and approval of the bedside team. eRT staff can contact the primary on-site team to suggest changes in care delivery but cannot enter any orders without the knowledge of the primary clinical team.
Earlier intervention, better cost-efficiency, improved procedures

The tangible success of the program is statistically documented in NEJM Catalyst: Innovations in Care Delivery and in the Journal of Clinical Medicine. From May 2020 through August 2021, 31,609 RT activities had been performed, 97.8% of which were related to the routine established workflows. Over 1,500 interventions – most occurring at night and on weekends – resulted in avoiding several near-miss events, and improved patient care, according to Krzysztof Laudanski, MD, PhD, assistant professor of anaesthesiology and critical care at the Hospital of the University of Pennsylvania. He and his colleagues attribute this to the ability of an eRT to intervene early, often before the bedside RT.
Penn Medicine estimates that US $79,095 was saved in staff cost during the 16 months of the study. An estimated US $119,391 in additional savings was attributed to costs avoided by the remote RTs not needing to use personal protective equipment (PPE), and by enabling on-site RTs to use their time more efficiently in dealing with the increased patient workload caused by Covid-19. Additionally, the eRT service detected unfavourable practice patterns in ARDS treatment and intervened before the ARDS electronic “trigger” was activated. In 2,685 cases the eRT service reduced harm to patients by aiding the implementation of a low stretch protocol in patients with ARDS, a protocol associated with a reduction in mortality and length of stay.
The eRT program is ongoing and greatly matured. A subsequent study is currently being conducted to investigate the optimal way to interact between eRT and bedside teams to assure the high reliability delivery of healthcare in ARDS, hyperoxia, extubation, and other targeted interventions using quantifiable improvement in patient care at a lower expenditure and burden to the staff.
Profile:
Krzysztof Laudanski, MD, PhD, is an assistant professor of anaesthesiology and critical care at the Hospital of the University of Pennsylvania. He is a Physician Lead at Penn E-lert for Quality and Implementation. Dr Laudanski works in the tele-ICU service and chairs the TeleICU Committee for the Society of Critical Care Medicine (SCCM). His research focuses on genetically driven and modifiable determinants of immunological recovery after burn, trauma, cancer surgery, Covid-19, and other critical care illnesses. He translates his projects in clinically oriented intervention for improved patient care, mentoring opportunities, and start-ups.
09.12.2022