Article • LTX overview
Lung transplant surgery: last hope for patients with advanced lung diseases
Despite treatment, chronic lung diseases such as COPD or cystic fibrosis can become so severe that a lung transplant is necessary. Dr Urte Sommerwerck explains which patients might be considered for transplantation and why follow-up is as important as the surgery itself.
Interview: Sascha Keutel
HiE: When is a lung transplant necessary?
Dr. Urte Sommerwerck: 'For a long time lung transplantation – LTX for short – was considered the last resort when all other treatment options had been used and the patient was at risk of dying from the lung disease within the next two years. This principle was extended to include a high likelihood of 90-day survival and of five-year survival with mortality due to accompanying diseases.'
Which requirements does a donor organ have to fulfil?
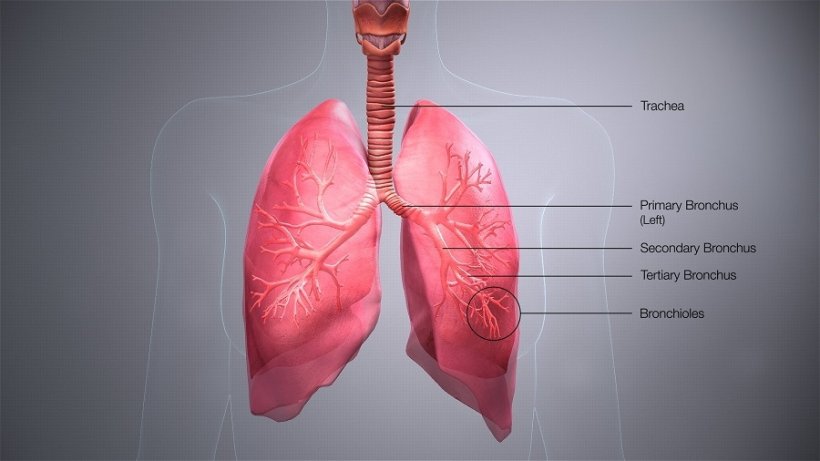
'The lung has permanent contact to the environment and can be injured, for example due to infections or ventilation. Thus it is an organ that is rarely transplanted. In addition, not every lung of the very few that are donated is suitable for transplantation.
'Luckily, modern normothermic ex-vivo lung perfusion (EVLP) allows us to better perfuse the lungs with an optimised electrolyte solution and thus improve the quality of the donor organ. This process has greatly expanded the pool of suitable organs and is the main reason why the number of lung transplants has been stable for the past couple of years despite organ donation scandals and the Corona pandemic. In Germany, an average of 300 lungs were translated per year over the past decade – which is still an extremely low number compared to other countries.'
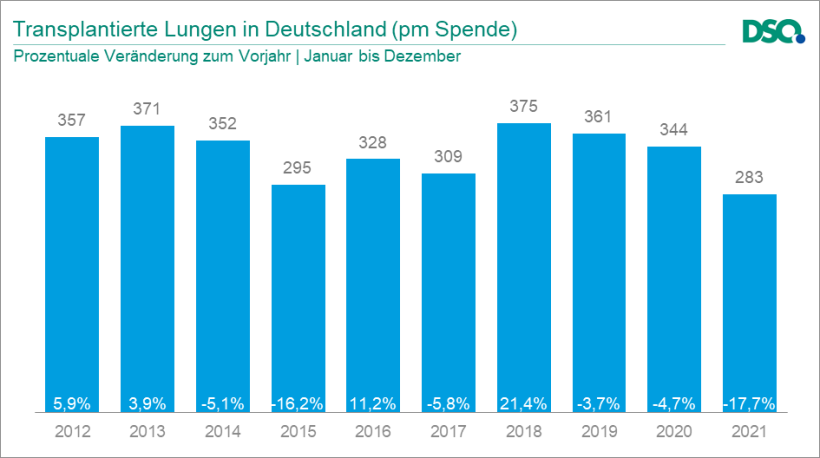
Image source: Deutsche Stiftung Organtransplantation (DSO)
How is a patient placed on the waiting list?
'In Germany, in order to be placed on the waiting list the patient has to present in one of the 16 lung transplant centres in the country. A 3-person board with the transplant pulmonologist, the surgeon and a further physician decide whether the patient will be placed on that particular centre’s waiting list. If a patient is refused, they can approach a different centre. If the patient is accepted, they are assigned a so-called Lung Allocation Score (LAS) between 0 and 100. This score takes into account the severity of the disease and the outcome prognosis. If the score is between 40 and 60 the transplantation will be performed within the next few months. A lower score means longer waiting times. Is the score above 60, the patients are often severely ill and already in intensive care – which diminishes the survival prognosis.
'These ethical considerations also apply to extracorporeal membrane oxygenation (ECMO). Patients who have been on a heart-lung-machine for a long time frequently don’t have a good prognosis; experience shows that positive transplantation outcomes are rare in these cases. Most patients are severely ill and suffer organ failure; they were not previously trained and screened in the transplantation programme. In addition, it can happen that information on previous diseases is incomplete.'
These patients are too ill?
'Exactly. Exclusion criteria for organ transplant surgery can be on both ends of the scale: the patient status might be too good or already too poor for transplantation. The ideal patient for transplantation, so to speak, is severely ill but still fulfils the strict criteria, and they have a post-surgery survival prognosis of at least five years.
'The Covid-19 pandemic has further limited these considerations since all of a sudden many healthy patients suffered from total lung failure and had to be moved to ECMO right away. Currently, it is being discussed whether these patients should also receive a transplant if there is no other regeneration option. But Covid is an infection and at this point we don’t know yet whether the transplanted organ will also be affected.'
Who decides which patient will receive a donor organ?
“The allocation of donor organs is exclusively based on medical and ethical considerations. A potential donor organ is registered with the German Foundation for Organ Transplantation, DSO. Eurotransplant, the organisational centre for the allocation of donor organs in eight affiliated European countries, is responsible for the actual allocation. It ensures that each organ is transplanted where it is most urgently needed.
'Unfortunately, Germany has a very small pool of donor organs. From a patient’s point of view it was therefore incomprehensible that in 2020 the German Parliament did not adopt the so-called double refusal solution. That approach considers every citizen a potential organ and tissue donor who did not explicitly refuse to be a donor during their life or whose closest kin do not refuse an organ donation. This approach is the current legal situation for example in Spain where you have 34 organ donors per 1 million inhabitants. In Germany, there are only 11.2 donors.
'In the end, the German Parliament adopted the so-called extended consent solution which mean organ and tissue removal is only allowed if the donor during their life or their next of kin consented.'
What is the survival rate after a lung transplant and which complications might occur?
'Obviously, the prognosis depends on the underlying disease. Nevertheless, transplantation follow-up is very important since the lung is an organ in constant communication with the environment: with each inhale viruses or bacteria can enter the body. Thus, from the very first day the patient body will try to stave off complications. Good chances for recovery require close cooperation between the transplant pulmonologist and the surgeon.
'The first few days post transplantation will be shaped by unstable blood pressure, hyperacute rejection reactions and intensive care, including ventilation. When the patients have survived the first few acute weeks and have been weaned off the ventilator so they can breathe by themselves, the next major challenge follows: in the first year post surgery the patients are on high doses of immunosuppressive medication in order to avoid rejection of the transplant. That means the body’s own immune system is suppressed and the stronger the immunosuppression the higher the probability of an infection.
'When the patient has survived the first year after the transplantation, immunosuppression will be significantly reduced. Now long-term rather than acute problems need to be managed properly. While the infection risk is sinking, the risk of acute and chronic rejection reactions and side effects of the immunosuppression remain. The immunosuppressive medications are incredibly toxic and can injure any organ. Renal insufficiency or malignant tumours are possible side effects which can appear years after the transplantation.'
What are the specific challenges caused by Covid-19?

'For the patients corona is obviously a particularly difficult challenge since they are high-risk patients. Some of them don’t react to the vaccination at all because they don’t have the necessary antibodies as the immune reaction is made impossible by the immunosuppressive regimen.
'Moreover, the patients lose years of their life due to corona. Unlike heart or kidneys, transplanted lungs have a limited life time. Patients gain five or six years with a lung transplant and now, due to the Covid pandemic, they can’t leave the house for more than two of those years.'
Profile:
Dr Urte Sommerwerck is Medical Director of the Department of Pulmonology, Allergology, Sleep and Ventilation Medicine the Augustinerinnen Hospital in Cologne, Germany. The former transplant pulmonologist at University Hospital Essen, Germany, is expert for lung transplantation with the audit committee of the German Medical Association.
01.11.2022