Article • Microarrays
Taking biomarker research to a new level
Harnessing the potential of digital pathology is taking research into new and more efficient biomarkers to a new level. By combining strategic planning with the latest digital pathology technology, high quality tissue microarrays for biomarker research are being produced.
Report: Mark Nicholls
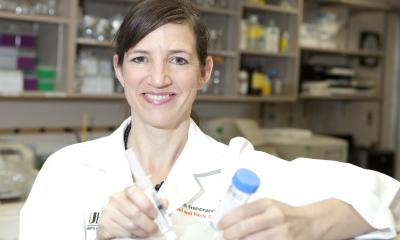
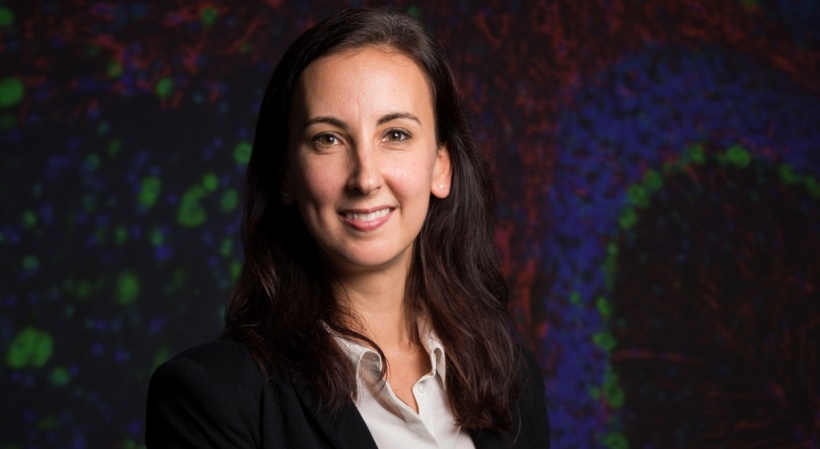
This December, at the Digital Pathology Congress in London, the application of digital pathology in this area was highlighted by Professor Inti Zlobec from the Translational Research Unit at the Institute of Pathology, University of Bern, in Switzerland.
Her presentation on the ‘Application of digital pathology to the construction of high-quality tissue microarrays for biomarker research: The next-generation tissue microarray (ngTMA) approach’ demonstrate how digital pathology can be applied to construction of tissue microarrays. ‘The inclusion of digital pathology into our tissue microarray workflow means we can have very high quality tissue microarrays that also allow us to address research questions we could have never answered before,’ she told European Hospital, ahead of the international meeting.
Zlobec explained that by using digital pathology constructing tissue microarray becomes more efficient and precise. In an example where a biomarker needs to be examined on 500 tissue blocks, small cores can be punched out from each tissue and repeatedly transferred into an empty paraffin block to produce a tissue microarray. ‘Tissue microarrays are a way of putting together an archive of all of these different patients material into one single block,’ she added.
Planning is a critical point
Before, we had to approximate from where we would be taking out those tissue cores, but now, because we have digital pathology, we know exactly which region we want transferred out from that block
Inti Zlobec
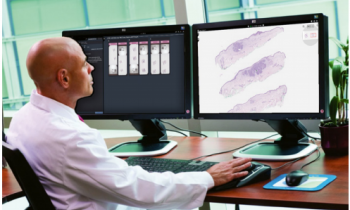
The process effectively creates a tissue microarray that contains dozens, or even hundreds, of different tissue cores, ranging in size from 0.6 to 2.0mm in diameter that contains selected regions for transfer into the TMA. ‘This would have been impossible without digital pathology,’ she confirmed. ‘Before, we had to approximate from where we would be taking out those tissue cores, but now, because we have digital pathology, we know exactly which region we want transferred out from that block.’
This is a ‘more specific, targeted and efficient’ approach. However, Professor Zlobec believes at Bern they take the approach one step further by defining their ngTMA approach by three pillars: planning and design; application to digital pathology; and automated tissue micro-arraying. ‘The planning phase makes or breaks the TMA quality, so regardless of how big the project size is – 10 patients or 1,000 – the planning is a critical point,’ she explained.
Examples of key questions to keep in mind are: does the research question require a targeted ngTMA approach or can it be achieved without digital pathology; what histological regions need to be captured to answer the research question; how many patients does the project need to achieve the required statistical power; and how many cores should you use to account for the possible heterogeneity in the tissue?
‘These are questions we never really asked before, when we did not have this new ngTMA approach,’ Zlobec added. ‘Once we have the plan and a corresponding slide we scan it, view it, annotate it, and finally align it with the actual tissue block from which it came. The annotated regions are cored out and transferred so, in the end, we have this amazing and precise ngTMA block, which can be cut and prepared for biomarker analysis.’
A whole new field awaits
The Bern team also creates ngTMAs of animal models of human disease for comparison. There are significant benefits for clinicians, researchers and patients. ‘On the one hand, we have an ngTMA approach that allows for high throughput biomarker screening and, on the other, allows us to go in-depth to answer targeted research questions that can only be addressed because we have this digital pathology aspect. ‘We can apply our approach to a large number of patients in a way that is very cost-effective and resource sparing in terms of tissues, consumables and time in the lab. ‘Because we can make these digital annotations on scanned slides we can construct ngTMA in a very precise manner and for the first time we can study important interfaces inside the tissue.’
Additionally, in cancer biomarker research, for example, intra-tumoural heterogeneity can be explored with ngTMA by annotating different regions within the tumour. Also, because the slides are digital, the pathologists can go back to the annotation and see what exactly was cored out from that block, ensuring high levels of quality control. Such use of ngTMA helps to create standards for biomarker research and, because tissues that are in- cluded in a block undergo the same experimental conditions, this means that variability from batch processing can be considerably reduced. ‘All of these aspects combined mean we achieve high quality biomarker research and validation that can hopefully be more effectively translated back into patient management,’ she said.
The next step – as well as challenge – is the quantification of the biomarkers using image analysis software to objectively measure the biomarkers, which in effect ‘opens a whole field of digital pathology research’.
Profile:
Inti Zlobec PhD is professor and head of the Translational Research Unit at the Institute of Pathology, University of Bern, where she is involved in inter-disciplinary translational research that aims to improve the clinical management of patients with colorectal cancer. Her research also focuses on histomorphological biomarkers as prognostic and predictive features of tumour response to therapies.
23.05.2016