Surgery proves successful for Type 2 diabetes remission
Obesity is physically debilitating – and costly for healthcare. Losing excess weight has positive effects on the entire metabolism and improves life expectancy. However, for patients who cannot lose their morbid, excess weight through diet, today’s surgical interventions can help towards permanent weight loss – and reduction in insulin dependency for diabetics.

Way back in 1950s accidental observations and reports showed that it is possible to reduce the insulin dependency amongst Type 2 diabetics by bypassing the duodenum. Dr Michael Frenken was the first doctor in Germany to operate on Type 2 diabetics with the primary objective of achieving diabetes remission. By bypassing the duodenum during the digestive process and the passage of food it was possible to reduce the insulin dependency of Type 2 diabetics. His results confirmed earlier observations. However, the type of surgical procedure, the length of the disease and the period of time for which the patient has been dependent on insulin are all significant factors for a complete remission.
Dr Frenken, who is a now a consultant at the Department for General, Visceral and Transplant Surgery at University Hospital Heidelberg, hopes that a prospective, randomised and controlled multicentre study, led by the University, and involving arround 400 people, and beginning in mid-2012, will confirm his observations. Since 2005, Dr Frenken has operated on 142 patients with Diabetes mellitus Type 2 at the hospital in Monheim. 90% of these patients were morbidly obese (BMI over 35), 10% had a BMI under 35 and were therefore, according to current legislation, not entitled to weight-reducing surgery because of morbid obesity. 82% of patients who had the surgery were insulindependent. This is the largest study series published in Germany so far.
Dr Frenken used three types of weight-reducing surgery for his interventions, i.e. the very popular gastric bypass (for 31 patients), biliopancreatic diversion, also known as the Scopinaro procedure (for 17 patients), and biliopancreatic diversion with duodenal switch (for 94 patients). The result was a dramatic improvement of the Type 2 diabetes within only a few days after surgery at a point where patients had not yet started losing weight. The reason for this is not yet clear; most probably the improvement of blood glucose levels can be traced to specific hormonal changes that occur after bypassing the duodenum, and which happen very quickly – but are, in principle, also reversible.
What are the predictors of success?
Not all patients who underwent surgery were free of diabetes afterwards. However, based on Dr Frenken’s examination results it is now possible to predict relatively well who might benefit from the surgery, i.e. gain a complete remission. However, even patients who do not achieve a complete remission can benefit considerably from surgery. The most successful procedure has been shown to be biliopancreatic diversion (BPD) in both its versions. Even patients who have been insulin-dependent for 5-10 years achieve a 90% remission. Only 50% of patients undergoing a gastric bypass achieve those results. Patients who have been insulin-dependent for less than five years achieve a remission quota of 80% after gastric bypass surgery and of 95% after BPD.
However, if patients have been insulin-dependent for more than 10 years the insulin producing cells in the pancreas are so burnt out that a complete cure for these patients -- or to alleviate the insulin dependency completely -- is usually no longer possible. The remission rate after BPD then drops down to 50% and after gastric bypass to considerably lower than 50%.
Another possible argument for biliopancreatic diversion as the procedure of choice to treat Type 2 diabetics patients who have been insulin-dependent for longer is that the recurrence rate after gastric bypass is up to 40% after five years, but after BPD it is only a maximum of 4% in a much more diseased patient population.
The explanation for this may be that after gastric bypass surgery the remaining beta cells are stimulated into increased insulin production because there is still an insulin resistance, even though this is much improved, whilst after BPD there is literally a recovery of the beta cells because this type of surgery facilitates a complete
recovery of inulin sensitivity.
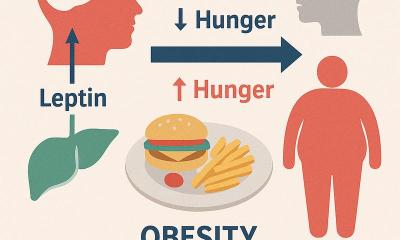
The decisive feature of Type 2 diabetes is that patients have an insulin resistance, i.e. although they initially produce sufficient insulin, the peripheral organs, particularly the liver, as well as fat cells and muscles do not recognise the insulin signal properly and the body has to produce more insulin for the glucose to be metabolised appropriately.
In the development of Type 2 diabetes there is the initial insulin resistance, which is compensated for quite a long time by increased insulin production, up to the point where this compensation mechanism no longer works. From a certain point the pancreas can then no longer produce increased amounts of insulin and, from then on, patients slowly develop into manifest Type 2 diabetics. Their blood sugar levels increase and that raised blood glucose level has a toxic effect on the pancreas, with continued destruction of the insulin producing cells functionality in the pancreas.
The soon to begin multicentre study will show evidence, at the highest level, as to whether the expectations generated by Dr Frenken’s results in Monheim are justified. ‘If, eight years after the start of the study, we can show that through surgery it’s possible to lower the mortality rate as well as the rate of diabetic complications in Type 2 diabetics, then this will be a breakthrough for this procedure,’ he concludes.
30.04.2012