Study finds gene mutations sensitize tumors to specific cancer drugs
Mutations in ARID1a, which are common in many cancer types, disrupt DNA damage repair in cancer cells, allowing the cancer to progress. This gene may also be an Achilles' heel when treating certain tumors, according to a team of researchers at The University of Texas MD Anderson Cancer Center.

The study, published in Cancer Discovery, discovered that certain mutations in ARID1a (AT-rich interactive domain-containing protein 1a), a gene recently implicated in cancer progression, sensitize some tumors to PARP inhibitor drugs, such as olaparib, veliparib and BMN673, which block DNA damage repair pathways.
"Our results showed, particularly in the ARID1a deficient cells, PARP inhibitors are more effective than in other cancer cells," says Guang Peng, M.D., Ph.D, assistant professor, Clinical Cancer Prevention, and senior author of the study. "Based on the mechanism we've discovered, we propose a new approach for targeting these mutant cancer cells."
According to The Cancer Genome Atlas, ARID1a is frequently mutated across many cancer types, and is the most commonly mutated gene in a subset of ovarian cancer known as clear cell carcinoma, with over 50 percent of tumors containing gene alterations. High ARID1a mutation rates are also found in uterine endometrioid carcinoma, gastric cancer, hepatocellular carcinoma and breast cancer, among others.
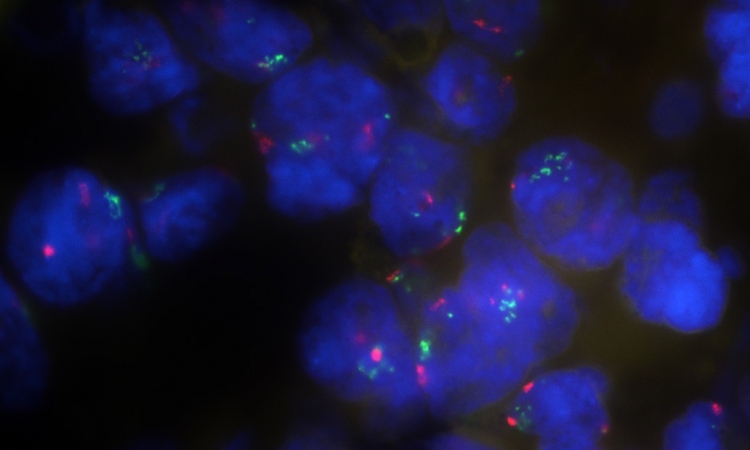
ARID1a is a component of the SWI/SNF complex, a group of proteins that work to rearrange the structure that organizes DNA, known as chromatin. This complex is also important for reorganizing this structure when DNA is damaged, so that cellular machinery can make repairs. When ARID1a is lost or mutated, cancer cells lose some ability to sense and correct DNA damage.
In this study the team identified, for the first time, the precise mechanism by which ARID1a plays a role in DNA damage response. Their findings revealed that it interacts with ATR, a protein with well-known roles in damage repair, and helps organize the DNA structure at the damage site.
Without normal ARID1a function, DNA damage repair is not performed as efficiently, and cancer cells are more sensitive to therapies that further disrupt critical repair pathways, such as PARP inhibitors. Using cancer cell lines as well as mouse models, the team showed that PARP inhibitors are significantly more effective at killing tumor cells with ARID1a loss or mutation.
The findings add ARID1a to a group of genes including BRCA1 and BRCA2 that confer a selective lethality to PARP inhibitors when mutated.
This represents what could be a major therapeutic target, particularly for clear cell carcinoma patients where standard treatment is not as effective as in other ovarian cancer subtypes, explains Peng. The study highlights the importance of using genomic information to guide cancer therapy and identify more precise treatments for individual patients.
However, not all ARID1a mutations are created equal and not all will impact its functions in the same way.
"We need to identify which regions of this protein are critical for DNA damage response and repair, as not all patients with ARID1a mutations will be sensitive to PARP inhibitors," says Peng.
Their future work will focus on classifying those mutations as well as identifying other ways to selectively target cells with mutations in ARID1a or alternate members of the SWI/SNF complex.
Source: University of Texas M. D. Anderson Cancer Center
12.06.2015