Malaria Treatment
Soon to be Simpler, More Flexible, and More Efficient?
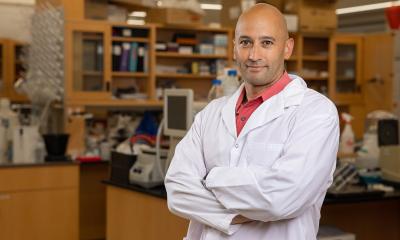
Malaria infections may soon be treated much more efficiently than they are at present. Researchers at the Universities of Bayreuth and Jerusalem have developed a novel drug release procedure for this purpose. The procedure enables the active ingredient Artemisone to be administered reliably at quantities and time intervals that are tailored exactly to the patients’ individual needs. The scientists have published their findings in the journal Global Challenges. This research was part of a project which received a total of around 1.5 million euros in funding from the German Research Foundation (DFG) over a period of five years.

Reliable and flexible: achieving the optimal dosage via tiny fibres
To be able to adapt the course of malaria treatment flexibly to fit the individual needs of the patient, the scientists placed the substance Artemisone on special polymer fibres that are around 100 times thinner than a human hair. The Artemisone is gradually released once it comes into contact with a standard infusion fluid containing surfactants. The size of the Artemisone dose that enters the patient’s bloodstream is easy to regulate. The fibres from which the Artemisone molecules are gradually released never make it into the patient’s bloodstream. Rather, they remain fixed to a drip chamber attached to the bottom of the fluid container.
This procedure represents a fundamental departure from previous approaches to the “programmed release” of anti-malaria drugs. Until now, research had focused on how to control drug release within the patient’s body. In particular, implants and special encapsulation techniques in pills had been investigated. “All of these approaches ran into difficulties that could not be overcome to date. Our procedure is unique in that it shifts drug release to an earlier stage. It takes place in the infusion system and thus entirely outside the patient’s body”, Prof. Dr. Andreas Greiner of the University of Bayreuth explained. “We are thus able to avoid all the uncontrollable health risks that could arise when a drug carrier is kept in the body for an extended period of time, being gradually released from inside the patient’s body,” explained doctoral researcher Amir Reza Bagheri (M.Sc.), whose research in Bayreuth in the field of polymer science played a significant role in these findings.
The scientists who developed the anti-malaria procedure stress that the tiny polymer fibres are also well-suited to serve as vehicles for other drugs, and could thus facilitate the treatment of other diseases as well.
No longer just a utopian vision: effective treatment for malaria patients in the tropics
The treatment procedure ties in with experiments being carried out at other research institutions that have been achieving promising results by testing Artemisone. “Preclinical tests have shown that Artemisone has clear benefits compared to the drug Artemisin, which is currently used to treat malaria infection. That is why we chose to concentrate on this more efficient active ingredient – an Artemisinin derivative, chemically speaking – from the very beginning in the development of our treatment procedure,” Prof. Dr. Jacob Golenser of the Hebrew University of Jerusalem explained. He is optimistic that Artemisone will be approved for treatment of malaria infections in the not-too-distant future. “Our infusion system is also expected to pass the required clinical tests. After that, there will no longer be anything standing in the way of applications in medical practice,” Prof. Dr. Seema Agarwal of the University of Bayreuth said.
Will the anti-malaria procedure developed in Bayreuth and Jerusalem be accessible to developing and emerging countries? The required fibres are produced via the electro-spinning of fleece: a routine industrial process. Covering the fibres with Artemisone and installing them in the drip chamber of an infusion set will not result in excessive costs, according to the scientists in Bayreuth and Jerusalem. “The infusion sets prepared in this way could definitely be affordable in developing and emerging countries where treatment of malaria infections is often lacking. If hospitals and malaria stations are equipped with standard infusion techniques, their patients may soon be able to receive efficient treatment,” Prof. Golenser predicts.
Source: Chair of Macromolecular Chemistry II, University of Bayreuth
20.03.2017