Image source: Cassiopeia_Arts from Pixabay
News • Autoimmune reaction study
Severe Covid-19 linked to increase in self-attacking antibodies
Hospitalized Covid-19 patients are substantially more likely to harbor autoantibodies — antibodies directed at their own tissues or at substances their immune cells secrete into the blood — than people without Covid-19, according to a new study.
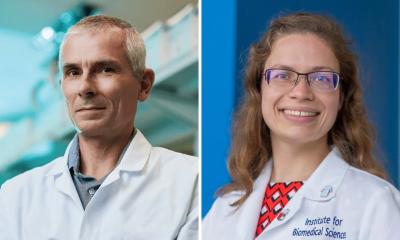
Autoantibodies can be early harbingers of full-blown autoimmune disease. “If you get sick enough from Covid-19 to end up in the hospital, you may not be out of the woods even after you recover,” said PJ Utz, MD, professor of immunology and rheumatology at Stanford Medicine. Utz shares senior authorship of the study, which was published in Nature Communications, with Chrysanthi Skevaki, MD, PhD, instructor of virology and laboratory medicine at Philipps University Marburg in Germany, and Eline Luning Prak, MD, PhD, professor of pathology and laboratory medicine at the University of Pennsylvania. The study’s lead authors are Sarah Chang, a former technician in Utz’s lab; recent Stanford undergraduate Allen Feng, now a technician in the Utz lab; and senior research investigator Wenshao Meng, PhD, and postdoctoral scholar Sokratis Apostolidis, MD, both at the University of Pennsylvania.
Within a week after checking in at the hospital, about 20% of these patients had developed new antibodies to their own tissues that weren’t there the day they were admitted
PJ Utz
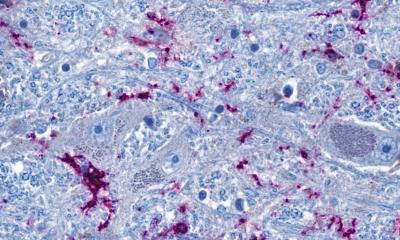
The scientists looked for autoantibodies in blood samples drawn during March and April of 2020 from 147 Covid-19 patients at the three university-affiliated hospitals and from a cohort of 48 patients at Kaiser Permanente in California. Blood samples drawn from other donors prior to the Covid-19 pandemic were used as controls. The researchers identified and measured levels of antibodies targeting the virus; autoantibodies; and antibodies directed against cytokines, proteins that immune cells secrete to communicate with one another and coordinate their overall strategy.
Upward of 60% of all hospitalized Covid-19 patients, compared with about 15% of healthy controls, carried anti-cytokine antibodies, the scientists found. This could be the result of immune-system overdrive triggered by a virulent, lingering infection. In the fog of war, the abundance of cytokines may trip off the erroneous production of antibodies targeting them, Utz said. If any of these antibodies block a cytokine’s ability to bind to its appropriate receptor, the intended recipient immune cell may not get activated. That, in turn, might buy the virus more time to replicate and lead to a much worse outcome.
For about 50 patients, blood samples drawn on different days, including the day they were first admitted, were available. This enabled the researchers to track the development of the autoantibodies. “Within a week after checking in at the hospital, about 20% of these patients had developed new antibodies to their own tissues that weren’t there the day they were admitted,” Utz said. “In many cases, these autoantibody levels were similar to what you’d see in a diagnosed autoimmune disease.”
Recommended article
News • Deadly mechanism uncovered
Inside COVID-19's 'cytokine storm'
Leading immunologists in Japan are proposing a possible molecular mechanism that causes massive release of proinflammatory cytokines, or a cytokine storm, leading to the acute respiratory distress syndrome (ARDS) in COVID-19 patients. Their suggestions, published in the journal Immunity, are based on recent findings that explain how SARS-CoV-2 enters human cells.
In some cases, the presence of those newly detected autoantibodies may reflect an increase, driven by the immune response, of antibodies that had been flying under the radar at low levels, Utz said. It could be that inflammatory shock to the systems of patients with severe Covid-19 caused a jump in previously undetectable, and perhaps harmless, levels of autoantibodies these individuals may have been carrying prior to infection. In other cases, autoantibody generation could result from exposure to viral materials that resemble our own proteins, Utz said. “It’s possible that, in the course of a poorly controlled SARS-CoV-2 infection — in which the virus hangs around for too long while an intensifying immune response continues to break viral particles into pieces — the immune system sees bits and pieces of the virus that it hadn’t previously seen,” he said. “If any of these viral pieces too closely resemble one of our own proteins, this could trigger autoantibody production.”
The finding bolsters the argument for vaccination, he added. Vaccines for Covid-19 contain only a single protein — SARS-CoV-2’s so-called spike protein — or the genetic instructions for producing it. With vaccination, the immune system is never exposed to — and potentially confused by — the numerous other novel viral proteins generated during infection.
We can’t say yet that you’ll definitely get an autoimmune disease — but you certainly might. I wouldn’t want to take that chance
PJ Utz
In addition, vaccination is less intensely inflammatory than an actual infection, Utz said, so there’s less likelihood that the immune system would be confused into generating antibodies to its own signaling proteins or to the body’s own tissues. “Patients who, in response to vaccination, quickly mount appropriate antibody responses to the viral spike protein should be less likely to develop autoantibodies,” he said.
Indeed, a recent study in Nature to which Utz contributed showed that, unlike SARS-CoV-2 infection, the Covid-19 vaccine produced by Pfizer doesn’t trigger any detectable generation of autoantibodies among recipients. “If you haven’t been vaccinated and are telling yourself, ‘Most people who get Covid get over it and are OK,’ remember that you can’t know in advance that when you get Covid-19 it will be a mild case,” Utz said. “If you do get a bad case, you could be setting yourself up for a lifetime of trouble because the virus may trip off autoimmunity. We can’t say yet that you’ll definitely get an autoimmune disease — we haven’t studied any patients long enough to know whether these autoantibodies are still there a year or two later, although we hope to study this — but you certainly might. I wouldn’t want to take that chance.”
Utz intends to study blood samples from SARS-CoV-2-infected people who are asymptomatic or who’ve had mild Covid-19 symptoms. That could help determine whether the massive hyperactivation of the immune system, which doesn’t occur in mildly symptomatic or asymptomatic people, is what causes trouble, or whether the mere molecular resemblance of SARS-CoV-2 proteins is enough to trigger autoantibody generation.
Source: Stanford School of Medicine
15.09.2021