Quality reporting for the MRI Quality Register
Young doctors' enthusiasm produces a valuable source of data on cardiac interventions
The German MRI Quality Register resulted from cooperation between the Department of Cardiology (headed by Professor Udo Sechtem) at the Robert Bosch Hospital in Stuttgart and the Elisabeth Hospital in Essen (Headed by Professor Georg Sabin).

The Institute of Medical Informatics and Biomathematics at Heidelberg University in Ludwigshafen, collects the data, and Heiko Mahrholdt MD, in Stuttgart, and Oliver Bruder MD, in Essen, are responsible for keeping the register.
In an interview with Daniela Zimmermann of European Hospital, Dr Bruder explained that The Institute for Heart Attack Research at Heidelberg University, in Ludwigshafen, supervises cardiac studies all over Europe via a protected, online entry system for all participating centres, and then statistically evaluates all the collected data for the Cardio-MRI Quality Register. ‘The main objective is to document who carries out what type of MRI in Germany in cardiology. There are further questions, such as what is the quality like, how safe is the procedure and which therapeutic consequences result from the findings of these examinations. What surprised us quite a lot was that, during the pilot phase, in the first year we already had 15 centres with more than 2,500 patients participating after only one e-mail request. This is remarkable because the number is significantly higher than for registers that are paid for per patient.’
Asked who, apart from medical insurers, needs this information, Dr Bruder pointed out that the statutory medical insurers are ‘only interested because the MRI working groups are all quite young, very active and very motivated. They are interested in the procedure itself, which is not something that can always be said for other registers. These young doctors enter the information in their spare time, they don’t mind doing it. They want to know who carries out MRI, how it is done and what the results are. For instance, we can see how many cardiac catheterisations don’t need to be carried out because of MRI diagnostics, and which additional type of diagnosis is required after MRI examinations. And we can also see if anything untoward happens. We work without exposure to radiation but use pharmacological stressors such as MRI contrast media for instance. This is an area where we are particularly interested in the safety aspect. We have realised that the acceptance of the register is high, that the safety is high and that the therapeutic consequences are very comprehensive: only a minority of examinations has no immediate benefit.
‘In the second phase of the register we would like to transform the whole project into a prognostic register, having confirmed in phase one that MRI is being used sensibly across Germany. During this second phase we’d like to gain prognostic data and to find out if the clinical path, such as carrying out a stress-MRI, for example, and then not proceeding with a cardiac catheterisation if there are no suspect findings, or to proceed with it if the stress MRI shows up pathological results, is the right way of doing things. We will be able to do this as we should have data about the one-year prognosis by then, and much as with other methods, we should be in a position to gauge whether patients with inconspicuous stress-MRIs have a good prognosis or not. We think they do, but so far we have not been able to confirm this with large numbers of data.
‘So the register will ensure that the procedure, which is already widespread, will be established within clinical routine even further. We will be able to deliver relevant data regarding safety. If, thanks to industry, we can increase the number of patients captured by the register to 10,000 and can then confirm that 9,000 of these had inconspicuous stress-MRI results with an excellent prognosis, this would be a clear reason why these patients should not have to undergo cardiac catheterisation. However, these data are currently not available for any of these examinations. Achieving this would constitute a real milestone, something that we have all been waiting for — and this can only be achieved through multi-centre studies, or registers, because they deliver the numbers and registers deliver the objectivity, because they are taken straight from daily, clinical experience.
‘The results will have an impact on medical insurers, and others, but mainly on hospital management and on clinical pathways. This procedure is not so catchy and cannot be described with statements such as ‘We will carry out fewer cardiac catheterisations’ or ‘We have a machine that replaces all this’. What we can say is that we have a system that can excellently carry out risk-stratification and can steer patients away from, or to, cardiac catheterisation in a much more controlled manner.’
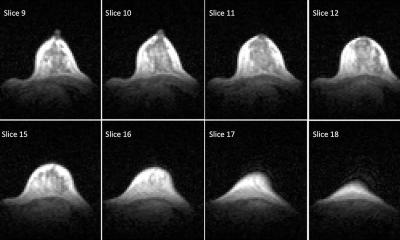
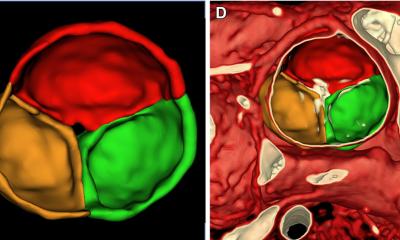
For MRI, he said, from a scientific viewpoint they are mainly interested in two procedures: late enhancement, which can show the accumulation of contrast media within scar tissue of the myocardium. First studies have shown that imaging this scar tissue – possible in this way and with this type of spatial solution only with MRI – is far superior to other prognosis parameters, such as heart muscle function and impairments of myocardial wall motility. This is one aspect that we can now demonstrate on a grand scale: a scar is more important than function and is an independent prognostic parameter.’
The second interest is in ischaemic diagnostics using the stress-MRI. ‘What we can show is that inconspicuous stress-MRI results constitute a good prognosis, and that those patients don’t really need cardiac catheterisation, because their life expectancy is the same as for those with a healthy heart. Nuclear medicine has problems with radiation exposure; there is prognostic data for many patients from registers, which show what we are now trying to prove with MRI. But we can then offer a procedure that doesn’t involve exposure to radiation, which we can repeat however often we want, without endangering the patient. This is a very important point. Also, nuclear medicine works with a spatial solution that is 30 to 40 times worse than ours. We are interested in the hard facts regarding circulation. What is the prognosis after one year – are there problems with circulation, yes or no. Is there a scar – yes or no. Large/small scar – yes or no. These are very simple questions. But the difference is whether you are looking at 5,000 patients or just 100. This is the point. The register, unlike a study, shows real world conditions. Everyone is included, whether they are comparative or not. Most studies state something like, patients under the age of so-and-so, or over the age of so-and-so were excluded, obese patients were excluded, women are often excluded when studies involve radiation exposure and in the end conclusions are drawn for the general public from a very restricted pool of study participants. Registers are different, amongst other reasons because they are more objective and because there isn’t anyone looking for and/or trying to engineer particular data. They are simply about total numbers. And it seems to be working, seeing how young doctors have enthusiastically got to work on it.’
30.04.2008