Image credit: John A. Rogers/Northwestern University
News • In utero monitoring during surgery
New probe tracks baby's health in the uterus
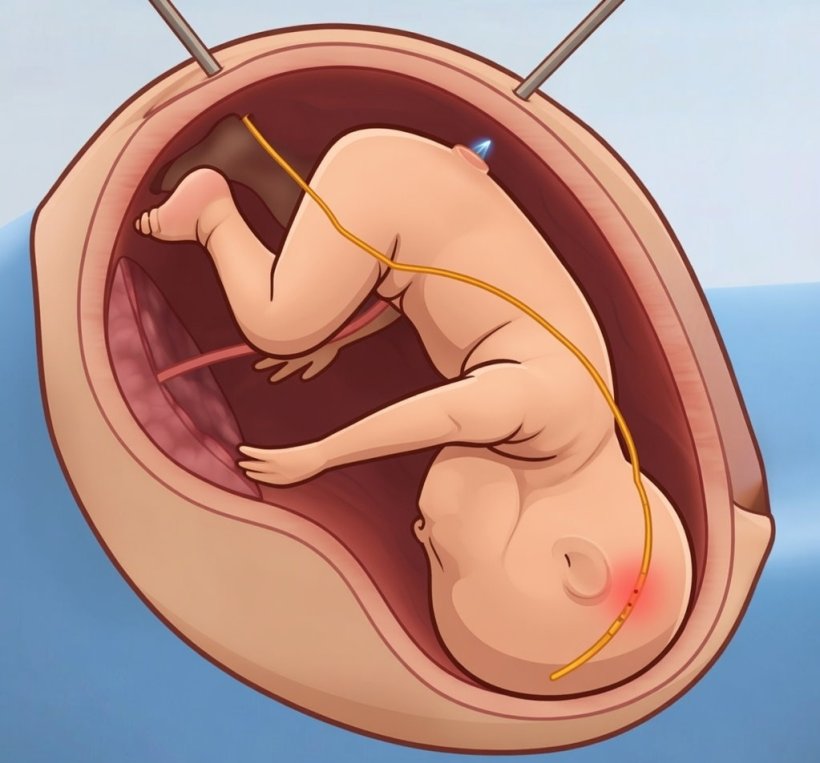
Flexible, hair-like device safely enters the uterus for continuous, real-time monitoring
Northwestern University researchers have developed the first device that can continuously track a fetus’s vital signs while still in the uterus — a feat that previously has not been possible.
The soft, flexible, robotic probe could dramatically improve safety during fetal surgeries, procedures in which physicians operate on a fetus before birth. Currently, doctors primarily rely on intermittent measurements of fetal heart rate using ultrasound imaging from outside the pregnant person’s body. The new device, on the other hand, can be gently inserted through the same narrow port already used in fetal surgeries.

Image credit: John A. Rogers/Northwestern University
Once inside the uterus, the device maintains stable, gentle contact with the fetus to reliably track heart rate, heart rate variability, blood oxygen levels and temperature. In studies on a large animal model, the probe provided accurate, precise, clinical-grade measurements even as the uterus and fetus moved during surgery. By tracking multiple vital signs simultaneously, surgeons gain a more complete and earlier picture of fetal distress, enabling faster interventions in case complications arise.
The study is published in the journal Nature Biomedical Engineering. It marks the smallest platform developed to date that is capable of accurately measuring vital signs.
Northwestern bioelectronics pioneer John A. Rogers led the device development in collaboration with Dr. Aimen Shaaban, a fetal surgeon at Ann & Robert H. Lurie Children’s Hospital of Chicago. The work builds on Rogers’ growing suite of soft, flexible devices designed to monitor the health of tiny, vulnerable patients, including premature infants in the neonatal intensive care unit (NICU). “Initially, Dr. Shaaban reached out to our lab to ask if we could adapt our vital signs monitoring systems for premature babies and apply them to fetuses during surgery,” Rogers said. “Right now, clinicians only have a partial picture of how a fetus is doing throughout surgery. We were presented with the challenge of designing a technology to monitor vital signs throughout the surgical process without creating an invasive access point or disturbing delicate tissues. Our flexible hair-like probe enters a port already used in minimally invasive fetal procedures and provides continuous, comprehensive monitoring without adding risk.”
Spina bifida [...] results in a lot of neurologic complications, including leg paralysis and hydrocephalus. Fetal surgery can reduce or even prevent these complications and can improve quality of life
Aimen Shaaban
“Performing fetal surgery with this sensor really shines a light on an area that’s been in the dark for so long,” Shaaban said. “When we operate on a baby after birth, we monitor a variety of parameters, including blood pressure, oxygen and carbon dioxide levels, heart rate and breathing. But for a fetus, who is more sensitive than a baby, we’re very limited. We don’t know what their vital signs are. Sometimes, the fetal heart rate drops during this procedure signaling low oxygen levels or a low blood pH. A slow fetal heart rate can develop abruptly and can even present with a full cardiac arrest for the fetus. Our ability to monitor the fetus hasn’t changed in 40 years. The tools just haven’t been there. We hope this probe provides multiparameter continuous monitoring of the fetus, enabling corrective adjustments at a very early stage to ensure fetal well-being throughout the procedure and avoiding any instability.”
Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering and Neurological Surgery at Northwestern, where he has appointments in the McCormick School of Engineering and Northwestern University Feinberg School of Medicine. He also directs the Querrey Simpson Institute for Bioelectronics and the Querrey Simpson Institute for Translational Engineering for Advanced Medical Systems. Shaaban is a pediatric and fetal surgeon at Lurie Children’s, professor of surgery and pediatrics at Feinberg and director of The Chicago Institute for Fetal Health. Rogers and Shaaban co-led the study with Yonggang Huang, the Jan and Marcia Achenbach Professor of Mechanical Engineering at McCormick and Hedan Bai, a former postdoctoral fellow from the Rogers’ lab and current assistant professor of materials at ETH Zurich.
In rare, complex cases, surgeons perform fetal surgery to correct life-altering or sometimes life-threatening congenital conditions before birth. One such condition is spina bifida, which affects thousands of babies each year in the U.S. Physicians also might perform fetal surgery to treat severe diaphragmatic hernias, urinary tract obstructions, fetal tumors or twin-to-twin transfusion syndrome, a serious complication in which blood flows unequally from one twin to the other. Surgeons perform these procedures as early as 15 weeks into a pregnancy. “Spina bifida is an opening in the spine that leaves the spinal cord and nerves exposed,” Shaaban said. “This birth defect results in a lot of neurologic complications, including leg paralysis and hydrocephalus. Fetal surgery can reduce or even prevent these complications and can improve quality of life.”
Over the past decade, surgeons increasingly have shifted from open fetal surgery — requiring a large incision into the uterus — to minimally invasive fetoscopic procedures, which use tiny instruments inserted through narrow surgical ports. While these less invasive approaches reduce risks for the pregnant patient, they also make it more difficult to monitor the fetus.
To address this challenge, the Northwestern team designed a slender, filament-like probe made from soft, flexible materials that can operate safely and gently inside the uterus. With a width just three times the diameter of a single hair, the probe is slim enough to pass through a standard tube already used during fetoscopic surgery, requiring no additional incisions. Once inside the uterus, soft robotic actuators enable the surgeon to guide and position the probe with precision. To ensure the probe stays in place, Rogers’ team designed a tiny, inflatable balloon-like cushion. The built-in cushion gently expands to hold the probe in stable contact with the fetus.
To optimize the probe’s shape, motion and contact forces, Huang and his former visiting Ph.D. student Xiuyuan Li used computational modeling to guide the devices mechanical design. “The device needs to gently press onto the tissue to form the kind of coupling needed to measure vital signs,” Rogers said. “Miniaturized balloons integrated onto the probe enable this coupling in a soft, minimally invasive manner. Our designs also use a similar mechanism to allow the filament to bend or twist, so that surgeons can robotically position it to a desired location.”
The team integrated multiple miniature sensors into the probe to simultaneously measure fetal heart rate, blood oxygen saturation and temperature. The device wirelessly transmits data to a monitor outside the body, providing surgeons with real-time feedback throughout the procedure.
By enabling continuous, multimodal monitoring, the new device could help surgeons intervene earlier or pause a procedure if a fetus shows signs of distress. It also could help give parents and caregivers more reassurance and peace of mind during anxiety-inducing surgeries. “When a pregnant mom needs a fetal operation, she places a lot of trust in her doctors to make sure that it is safe,” Shaaban said. “If we could give her more confidence that her baby will do well, that’s better for everybody. Anything we can do to make operations safer for mom and safer for the baby is a huge win.”
Source: Northwestern University
26.01.2026





