Photoimmunotherapy
Photo-Bombing Cancer
When Kerstin Stenson, MD, describes the innovative technique she is helping develop to fight cancer, it seems like she’s describing a Tom Clancy military espionage novel.
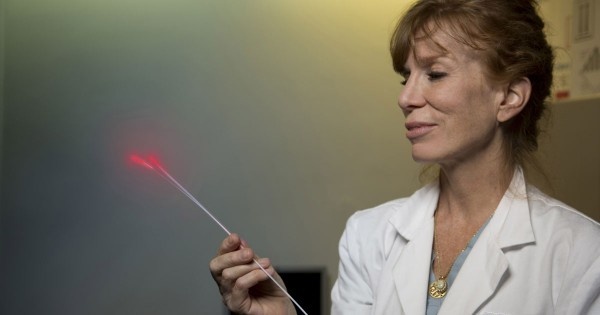
Stenson is treating patients with photoimmunotherapy, PIT for short, an experimental technique that combines the immune system’s ability to target cancer cells precisely with laser energy’s ability to destroy those cells. Like a high-tech weapon in a Clancy thriller, PIT delivers extremely precise, lethal payloads with minimum collateral damage.
“This treatment is so unique and promising because its cancer cell-killing power is so selective and immediate,” says Stenson, director of Rush University Medical Center’s Head and Neck Cancer Program. “It really is just like a guided missile.”
Cold war spy novels like Clancy’s that celebrate military technology aren’t Stenson’s first fiction choice, but she appreciates their parallels to her work when it comes to developing new weapons to fight an old enemy. Just as a hero needs to defeat the bad guys while also saving the hostages, PIT meets the fundamental challenge in defeating cancer: balancing the ability to destroy cancer cells while limiting the damage to surrounding tissue.
Delivering a payload, aiming a laser, and setting off an explosion
Photoimmunotherapy expands upon an existing therapy called photodynamic therapy, a two-step process that starts with a patient being injected with a specialized drug, called a photosensitizer, that’s designed to accumulate in and near a cancerous tumor. Then doctors beam specific wavelengths of light at the tumor, causing the absorbed photosensitizer to produce a form of oxygen which kills nearby cells.
But in photoimmunotherapy, the photosensitizer is combined with a laboratory-produced antibody — called a monoclonal antibody — that specifically targets and binds with receptors found only on the surface of head and neck cancer cells. Administered intravenously, the photosensitizer/antibody combination — referred to as a “payload drug” — circulates throughout the patient’s body, but only latches onto head and neck cancer cells.
The next day, Stenson affixes tiny, laser-optic fibers near the surface of the tumor. If the tumor is difficult to reach, she threads the fibers through small catheters directly into the tumor. Then the laser light energy is beamed through the fibers, hitting the photosensitizer target. The laser sets off molecular-level explosions that weaken the cancer cell walls, allowing water molecules contained in the surrounding tissue to rush in until cancer cells burst.
“Almost immediately, you can see the tumor start dying. It turns white and melts away,” Stenson says. Because the payload drug remains inert unless activated by a specific wavelength of light that doesn’t damage human tissue, destroying the cancer cells causes almost no damage to surrounding cells. “The drug/dye combination (the monoclonal antibody combined with the photosensitizer) is not toxic until activated by near infrared light, thus is very safe from a systemic perspective,” Stenson explains.
By comparison, patients treated with conventional photodynamic therapy, PIT’s predecessor, must avoid strong sunlight for several months because tiny amounts of photosensitizer that remain in their systems could be activated by the sunlight, causing a severe sunburn.
PIT provides option after other treatments have failed
Stenson is leading a clinical trial that is testing the safety and effectiveness of PIT for patients whose head and neck cancer is not responding to radiation or chemotherapy, or when surgery is not feasible due to a tumor’s hard to access location. “Getting inside the cancer cell means we can get systemic treatment locally more than any other treatment,” she says, adding that PIT is the most exciting and promising therapy she has ever been involved with.
The study is sponsored and funded by Aspyrian Therapeutics, the biotechnology firm that created the monoclonal antibody conjugate, RM-1929, and secured the exclusive license for the technology from the National Cancer Institute, which developed the original photoimmuno therapy technology.
“Photoimmunotherapy is a first-in-class treatment platform designed to provide an option for patients whose head and neck cancer has failed standard of care treatments,” says Merrill Biel, MD PhD, who developed the PIT clinical trial program and recruited Stenson and Rush to be one of the five participant sites in the safety and effectiveness study. “Chemo has not worked, radiation has not worked. Surgery can’t help them.” Rush is the only center in Illinois offering this treatment.
He asked Stenson to participate because of her national reputation in the field of head and neck cancer care. “She is known across the country for developing cutting-edge, innovative and life-saving treatments that advance our field and offer hope to patients who’ve run out of options,” he says. “Her expertise and insight have been a great addition.”
PIT could be treatment for other types of cancers
Beyond the exciting potential of PIT as a very effective therapy for head and neck cancer, it has great potential for treating other forms of cancer and as a combination therapy with immune-modulation chemotherapy. “We hope that once we prove the safety and effectiveness of this treatment specifically for head and neck cancer, the photosensitizer could be combined with immune stimulating drugs that target other forms of cancer,” Stenson says.
Because PIT therapy seems to work so precisely and quickly, there also may be great potential in combining the approach with surgery. Even when a cancer surgeon successfully removes a cancerous tumor, some cancer cells invariably remain in the surrounding tissue and are a danger to spread, which is why cancer surgery often is followed by chemotherapy. Since surgery makes those areas temporarily accessible, PIT’s one-two punch of light energy-activated targeted therapy might greatly reduce the chance that the cancer redevelops.
Source: Rush University Medical Center
07.12.2016