PET/CT Predicts Early Response to Chemotherapy
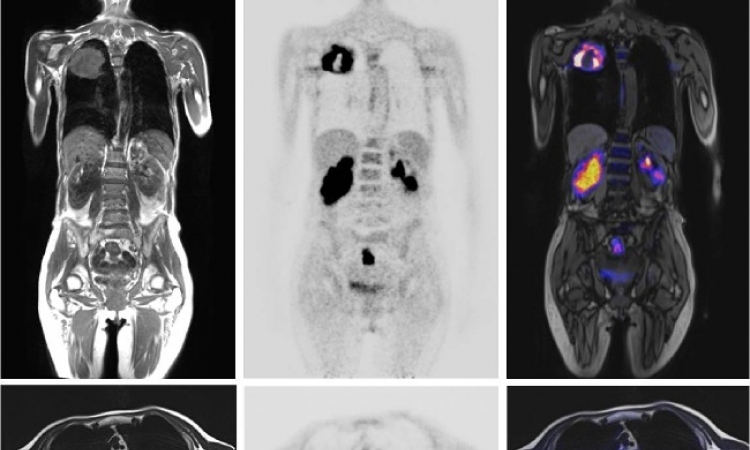
That wait time might be shortened for patients with soft-tissue sarcomas thanks to new research, from the Jonsson Comprehensive Cancer Center at the University of California, Los Angeles (UCLA), demonstrating that PET/CT can be used as early as one week after a single treatment cycle to determine whether the drugs are killing the cancer. Researchers made another surprising discovery—some tumors that actually grew in size responded favorably to chemotherapy.
Memorial Sloan-Kettering Cancer Center
The study, published in the April 2009 issue of Clinical Cancer Research, was conducted over a two-year period on 50 patients diagnosed with soft-tissue sarcomas. Patients received neoadjuvant chemotherapy to shrink tumors before surgery, according to Fritz C. Eilber, M.D., an assistant professor of surgical oncology who directs the Sarcoma Program at UCLA and senior author of the study.
The team used fluorodeoxyglucose (FDG) PET/CT scans to evaluate changes in the metabolism of glucose within the tumor compared with standardized uptake values. Cancer cells typically take up large amounts of FDG—a process that can be quantified on PET scans. A 35 percent reduction in the tumor's metabolic activity indicated a positive effect of chemotherapy on the cancer.
"It wasn't known how early the effect of the treatment would become evident, and there was a good chance that we wouldn't be able to tell for a while if it was working or not," said Dr. Eilber. "The thing that surprised us was that within just one cycle you could determine the effect of the treatment, and about half the patients weren't responding."
Of the 50 study participants, 28 showed no significant response in scans taken one week after the drugs were administered. "The quicker you can find out whether the drugs are working, the better off you are," said Dr. Eilber. "You can switch to a better drug or go to surgery because these are operable tumors."
Study Results Very Encouraging
These results are particularly significant because patients don't typically undergo a PET/CT scan until they are three months into chemotherapy, said Steven M. Larson, M.D., chief of the nuclear medicine service and the Donna and Benjamin M. Rosen Chair of Radiology at Memorial Sloan-Kettering Cancer Center in New York.
"It's an intriguing result and we look forward to seeing it validated in a larger series," said Dr. Larson. "Sarcoma is a very difficult disease to treat. Treatments have variable response, so if you can pick out a patient for whom a treatment is likely to work, it would be an important advancement. It's very encouraging."
Tumor Size May Not Indicate Treatment Efficacy
While reviewing images from the study, Dr. Eilber and the UCLA team made an observation they consider critical to metabolic responses in tumors—some tumors that responded to chemotherapy actually grew in size despite a decrease in FDG uptake.
That finding runs counter to current thinking that only tumors that shrink are considered to be responsive, said Dr. Eilber.
"The other surprise was that the tumor size on CT had no prognostic value at that early time," he said. "For example, let's say I do not remove one of the tumors and then I put the patient on a trial drug. Whether a patient is responding or not, and can continue the drug, depends on the tumor size. A lot of people who are actually responding to the drug would get taken off of treatment because they're not showing response by size criteria.
"In my opinion, they're missing a lot of responding patients by just using size as the standard," said Dr. Eilber. "If the tumor shrinks, that's usually an indication of response. Just because it doesn't shrink doesn't mean the tumor is not responsive. What PET allows you to do is accurately identify those patients who are truly responding."
Dr. Eilber said the protocol could easily be used at cancer centers worldwide due to the availability of PET/CT and through the use of commonly measured FDG uptake values.
Dr. Larson agreed. "There were about two million PET scans performed in the U.S. last year and that number is growing by 15 to 20 percent each year," he said. "That availability makes it likely that someone could have a PET scan anywhere in the country.
"FDG is our most standard tracer," he continued. "There are now radiopharmacies throughout the country that provide distribution. We're talking about widespread use of this nuclear medical tool having a big impact on clinical care. People will begin to implement it on a wider scale."
Patients Gain New Tool in Cancer Battle
Both physicians said it will be important to see reports on long-term outcomes for this patient cohort and to study larger patient groups as well. For now, Dr. Larson said this protocol could provide patients with another tool in their battle to preserve quality of life while fighting a potentially deadly disease.
"The issue here is the timeliness of response," said Dr. Larson. "Within a week or two, a physician can make a decision about a patient who does not need to be treated further with expensive drugs that have side effects. The patient can potentially seek alternative treatments which may be effective."
That is a considerable advantage in today's increasingly demanding healthcare environment, said Dr. Eilber.
"The idea of waiting to see if a treatment works just isn't good enough for patients these days," he said. "They're trying all kinds of things … molecular assays on tumors, dumping chemotherapy directly on tumor cells to see whether it kills them or not. They want to know outcomes fast. Not only does this method accomplish that, it's noninvasive."
PET/CT Sessions at RSNA 2009
The multisession course, "Case-based Review of Nuclear Medicine: PET/CT," will be held in conjunction with SNM on Thursday, Dec. 3 at RSNA 2009. The PET/CT sessions and their presenters are:
• Head and Neck Cancers, Michael M. Graham, M.D., Ph.D.
• Cancers of the Thorax, George M. Segall, M.D.
• Cancers of the Abdomen and Pelvis, Dominique Delbeke, M.D., Ph.D.
• Sarcoma/Melanoma/Lymphoma, Eric M. Rohren, M.D., Ph.D.
Source: www.rsna.org
26.11.2009