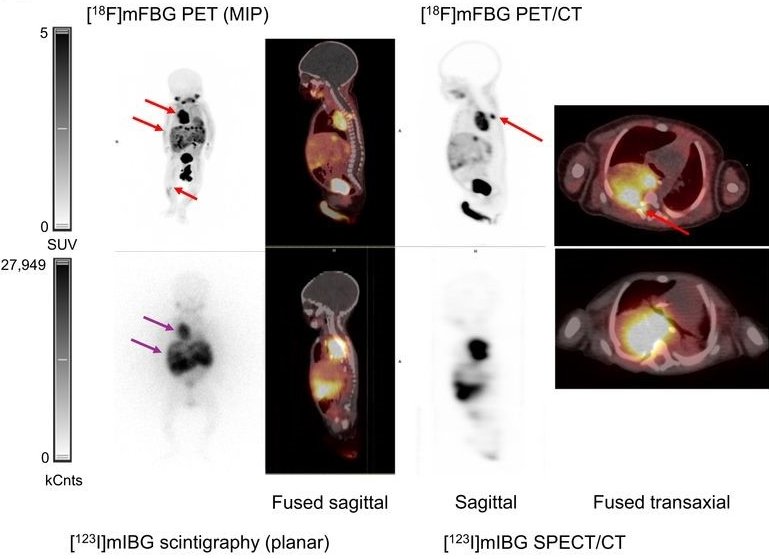
[18F]MFBG LAFOV PET/ULD CT (top) and [123I]MIBG scintigraphy with SPECT/LD CT images (bottom) of 7-week-old girl with neuroblastoma. [18F]MFBG image shows intraspinal and bone marrow involvement not seen on [123I]MIBG image. [18F]MFBG PET/ULD CT image shows uptake in tumor in right hemithorax with intraspinal involvement with direct extension into neural foramina and spinal canal between thoracic vertebrae 4/5 and 5/6 (top red arrow), several liver lesions (middle red arrow), and in bone marrow of right tibia (bottom red arrow). [123I]MIBG scintigraphy with SPECT/LD CT image shows only large thoracic tumor (top purple arrow) and liver metastases (bottom purple arrow). Spinal involvement and bone marrow involvement could not be identified on [123I]MIBG scintigraphy with SPECT/LD CT.
Image source: Borgwardt L et al., Journal of Nuclear Medicine 2024 (CC BY 4.0)
News • Neuroblastoma diagnosis without anaesthesia
New PET/CT technique improves brain tumour detection in children
A new molecular imaging technique that pairs a novel tracer with a next-generation PET/CT scanner can identify neuroblastoma in children with high sensitivity, requiring a scan time of only minutes and no sedation or anesthesia.
With its ability to accurately diagnose neuroblastoma, this technique, known as 18F-MFBG LAFOV PET/CT, has the potential to impact therapeutic decision-making for children with this disease. This research was published in the August issue of The Journal of Nuclear Medicine.
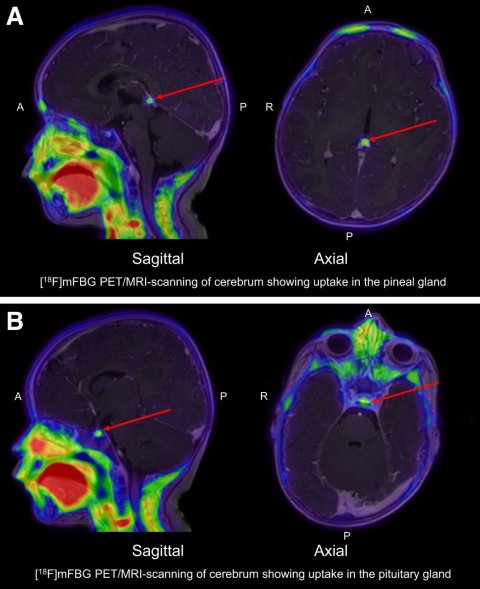
Sagittal and axial view of tracer uptake in pineal gland (arrows, A) and pituitary gland (arrows, B) seen on [18F]MFBG LAFOV PET/MRI. A = anterior; P = posterior.
Image source: Borgwardt L et al., Journal of Nuclear Medicine 2024 (CC BY 4.0)
Neuroblastoma is the most common extracranial solid tumour in children, with an overall survival of 70%. For decades, 123I-MIBG SPECT/CT has been the standard of care for initial staging, response assessment, and frequently used follow-up of neuroblastoma. The 123I-MIBG SPECT/CT scanning procedure is a two-day protocol. Sedation or general anaesthesia is frequently used because the patients are predominantly infants and due to the lengthy scan time, often more than two hours.
“For young children undergoing molecular imaging, less exposure to radiation and the avoidance of sedation or general anaesthesia is very important,” said Lise Borgwardt, MD, PhD, senior consultant in paediatric nuclear medicine at Copenhagen University Hospital-Rigshospitalet, in Copenhagen, Denmark. “In our study, we used the tracer 18F-MFBG which requires only a one-day protocol, at the long-axial-field-of-view (LAFOV) PET/CT scanner, which has a sensitivity about 10 times higher than a digital PET/CT scanner. We then compared this technique with 123I-MIBG SPECT/CT to determine its diagnostic value and feasibility.”
The fact that these scans can be performed without anaesthesia or sedation, and at a lower radiation dose is a big step forward for the children, parents, and the healthcare system in general
Lise Borgwardt
The study included 10 children with neuroblastoma who received 123I-MIBG SPECT/CT followed by 18F-MFBG LAFOV PET/CT. Masked readers independently scored the 123I-MIBG and 18F-MFBG scans for the presence of any pathologic lesions. SIOPEN and Curie scores (semi-quantitative systems used to assess metastatic disease burden) were also calculated.
None of the children required sedation or general anaesthesia with 18F-MFBG LAFOV PET/CT, whereas 80% had general anaesthesia with 123I-MIBG SPECT/CT. In addition, a PET acquisition time of only two minutes without motion artifacts was required for reconstruction to provide a clinically useful image with 18F-MFBG LAFOV PET/CT. Eighty percent of 18F-MFBG LAFOV PET/CT scans revealed more lesions than 123I-MIBG SPECT/CT scans and 20% revealed the same number of lesions. In 18F-MFBG LAFOV PET/CT scans, the SIOPEN score was higher in 50% of the cases, and the Curie score was higher in 70% of the cases. Intraspinal involvement, retroperitoneal lymph node involvement, and bone marrow involvement were diagnosed with much higher precision with 18F-MFBG LAFOV PET/CT.
“A scan with a much higher sensitivity can find very small lesions and the exact extension in the body and can be extremely beneficial in determining the right course of treatment,” said Borgwardt. “The fact that these scans can be performed without anaesthesia or sedation, and at a lower radiation dose is a big step forward for the children, parents, and the healthcare system in general.”
Source: Society of Nuclear Medicine and Molecular Imaging
23.08.2024