Paediatric radiology – a diagnostic tightrope walk
Paediatric radiologists are facing very special challenges. For their small patients they have to be able to precisely assess the advantages and risks of the different imaging modalities and procedures.

While for example CT on the one hand involves radiation which might be detrimental to the infant or child, it is on the other hand able to detect life-threatening conditions and might thus be crucial for the child’s survival.
Dr. Birgit Kammer, Senior Resident at the Department of Paediatric Radiology, Dr. von Haunersche Children’s Clinic at the University Hospital of Ludwig Maximilian University Munich, is well aware of the difficulties in paediatric radiology: “Many colleagues feel uneasy with these small patients and their severe conditions. But we paediatric neurologists need young talents. Our recruitment prob-lems are due in part to the level of compensation and in part to the fact that paediatric and adoles-cent medicine does not have a strong lobby.” As a particularly dedicated physician Dr. Kammer uses venues such as this year’s Bavarian Radiology Congress in Erlangen to spark interest by presenting challenging cases. Since her clinic enjoys nation-wide reputation as a highly specialized institution she can draw on her daily work: “Children from all over Germany come to us. Therefore we also see very rare diseases.” She knows that beyond the perimeters of a city like Munich diagnostic imaging facilities for paediatric patients are limited. Therefore her prime objective is to inform: she wants radiologists to be aware of the broad spectrum of paediatric diseases and she wants to help them diagnose these conditions properly.
In CT “good” means “diagnostic value”
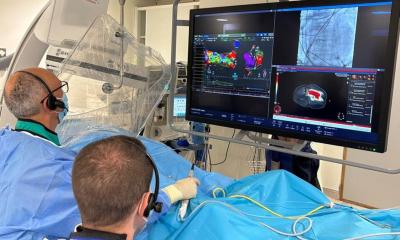
In paediatric radiology deciding on the suitable imaging modality is a tightrope walk. The radiologist has to answer several questions: Can CT provide a solid information base for a possible surgical intervention? Are contrast agents required and if so when and in which dose? How large a field of view is required? Is MRI the better modality even if the newborn has to be anaesthetized for about an hour? “With infants and small children MRI is difficult but it can be applied when a pulmonary sequestration, a double aortic arch and certain heart defects are suspected. CT however is always superior to MRI when visualization of the lung parenchyma and the airways is required, for example when a tracheal bronchus or a tracheal stenosis is present. Since malformations of the lung, the heart and the vessels are often – but not always – interconnected it may be a judgement call whether MRI or CT are preferred for diagnostic imaging,” Kammer explains.
What is to be taken into consideration when planning a CT exam of an infant who after all weighs only a few kilos? “The major objective is to acquire images that provide diagnostic information with-out harming the baby. Never ever apply the same protocols you would use for an overweight adult of 120 or 140 kilos!” the expert warns. Nevertheless the central goal of the exam – to detect malformations – must remain in focus: “No surgeon will agree to work on the thorax of a baby based on poor scans. That also means: If a CT has to be performed, don’t be afraid of the dose. As far as I am concerned that would be misunderstanding radiation protection. If your dose is too low and you can only suspect a pathology that does help neither patient nor physician.”
For Dr. Birgit Kammer a CT scan of an infant patient is a medical specialty which is indicated when serious conditions need to be clarified. But it does require an experienced radiologist. “Tracheal and lung malformations call for CT as do serious infectious lung diseases and the diagnosis of lung metastases. Many malformations can be better detected with CT than MRI,” Dr. Kammer sum-marizes her experience as a paediatric radiologist.
27.11.2012