MRI & Liver
MRI leading the way in metabolic disease imaging
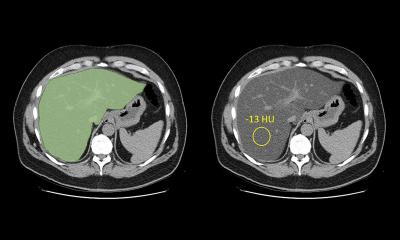
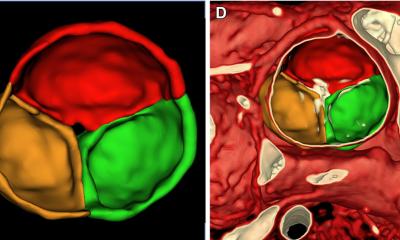
New MRI techniques are set to offer advances in the earlier detection of liver disease in patients. Radiologists are harnessing the potential of highly-targeted MRI, whilst exploring the imaging modality as a means of delivering non-invasive biomarkers, reducing the need for biopsy to measure treatment response.
Advances in this area are being outlined at the 17th International MRI Symposium in Garmisch in February by Professor Scott Reeder, Vice Chair of Research and Chief of MRI in the Department of Radiology at the University of Wisconsin.
In his presentation – MRI of the liver: metabolic diseases – he will highlight the growing use of MRI as a biomarker in a way to measure characteristics of the body, focussing on metabolic disease and metabolic syndrome.
While this topic covers “a full constellation of abnormalities”, he will specifically discuss diabetes and obesity and using MRI to measure features of those diseases, with particular emphasis on abnormal deposition of fat in the liver.
He explained: “Patients who are obese and have Type 2 diabetes will often have abnormal amounts of fat in the liver. However, the exact causal relationship is not entirely understood – whether fat is deposited because you have diabetes or whether fat actually contributes to the development of diabetes.”
Another issue, he said, is of central obesity - distribution of fat in the abdomen - and whether it is visceral fat or subcutaneous fat, factors which have implications for complications of obesity.
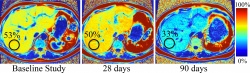
Over the last five years, there has been intensive development of non-invasive ways of quantifying those two disease features, with MRI a pivotal imaging tool in that with latest trends in this field pointing towards earlier detection of disease.
Professor Reeder said: “One of the complications of having fat in the liver is that patients would develop inflammation liver injury, fibrosis and even cirrhosis. Physicians are focussing more on earlier stages of disease, understanding that deposition of fat is abnormal, and if we can treat patients before they develop cirrhosis that is obviously a good thing.”
However, the development process has had its difficulties and challenges.
He explained: “One of the powerful aspects of MRI is that the signal depends on a large number of physical and biological determinants, and this is what also makes it such a rich modality where you can measure so many different things about tissue. Unfortunately, we must also account for many different factors that can confound our ability to quantify a specific tissue property.”
Such confounders include factors such as the type of scanner used, or the day the patient is scanned. Failure to account for the factors that impact on the signal when measuring liver fat can impact the accuracy of the measurement and - more importantly – “reproducibility”.
Understanding the physics of the process, he says, has been the biggest challenge, though he believes clinicians have now reached a point where they have “figured this out.”
Having refined the imaging methods, though with some clinical validation work still to be carried out, and gained more consistency through important understanding of the underlying physics, advances are now being made in how to use MRI in terms of metabolic disease in the realms of clinical care and drug development.
“There has been interest from pharmaceutical companies in using these as biomarkers instead of biopsies to measure treatment response,” he added. “My guess is that in another five years we will have a much better idea of how exactly these will be used in clinical care.”
Advances will see increased use of non-invasive imaging biomarkers potentially reducing the need for biopsy and the use of targeted MRI examinations – meaning less discomfort for patients but also providing more accurate results.
“Rather than doing an hour-long MRI we are going to be doing a 20-second MRI to answer very specific questions,” concluded Professor Reeder.
Profile:
Professor Scott Reeder is Vice Chair of Research and Chief of MRI in the Department of Radiology at the University of Wisconsin and Associate Director of the Medical Scientist Training Program in the School of Medicine and Public Health. He joined UW-Madison in 2005 from Stanford University where he completed his radiology residency, and a fellowship in abdominal and cardiovascular imaging. Originally from Canada, Professor Reeder is also the Director of the UW Liver Imaging Research Program, performing research in technical development and translation of new imaging methods, particularly quantitative imaging biomarkers, to assess liver disease. Specific areas of research interests include development of new MRI methods for quantification of abdominal adiposity, liver fat, liver iron overload and other features of diffuse liver disease.
03.03.2017