Article • Gynaecological radiology
MRI holds a key role in cervical cancer
Modern imaging techniques greatly enhance the treatment selection
Report: Michael Reiter

Staging of cervical cancer is clinically based on a system developed by the International Federation of Gynaecology and Obstetrics (FIGO). The staging is clinical because the majority of cases occur in developing countries where access to MRI is limited, explains gynaecological radiologist Dr Evis Sala. Clinical diagnosis is gained via a smear (pap test), clinical symptoms assessment and examination. Although MRI has been used for evaluation of disease extent in patients with cervical cancer for the last two decades, it was 2009 before FIGO acknowledged that, where available, CT and particularly MRI could be used to evaluate the extent of disease. According to the Dr Sala this is a key step forward regarding the use of imaging as part of the evaluation of disease extent in cervical cancer.
‘Imaging,’ she explains, ‘plays a crucial role in the patient journey. First of all, in young patients who wish to preserve fertility, there is an operation called trachelectomy: the cervix is removed and the tumour along with it, allowing preservation of the uterus. Studies have demonstrated that this method allows affected women to preserve fertility and carry a pregnancy to term. ‘Specialist surgeons capable of performing this procedure need the best information available to assess the patient’s eligibility. This is where MRI comes in. In almost 100% of cases, it is accurate in selecting patients suitable for trachelectomy and in achieving precise planning of that procedure.
‘Apart from fertility-sparing issues, triaging patients with cervical cancer is another purpose which MRI serves very well. If the tumour is small and has not spread into the adjacent parametrium, surgical removal of the uterus and adjacent tissue is performed. In cases where the tumour has spread to neighbouring tissues, radiotherapy is the appropriate option. Clinical staging has proved to be significantly inferior to MRI especially in the early stages of the disease spread to the adjacent tissues (parametrium).’
In general, functional MRI techniques such as perfusion and diffusion MRI provide insights into tumour biology, and quantification of changes following treatment is possible
Evis Sala
Speaking of other applications for MRI, Dr Sala pointed to the evaluation of tumour recurrence. ‘MRI can map out recurrence very nicely in the pelvis and the lymph nodes. MRI can be combined with PET/ CT if there is a question about distant metastases, for example, in the chest,’ she added.
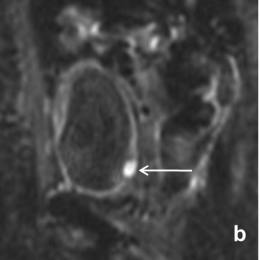
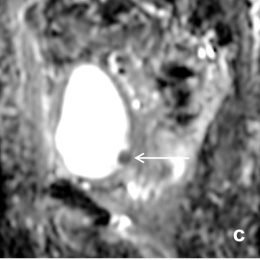
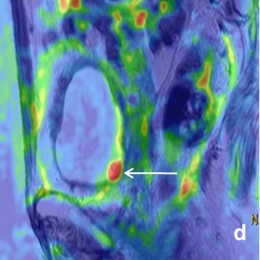
‘In general, functional MRI techniques such as perfusion and diffusion MRI provide insights into tumour biology, and quantification of changes following treatment is possible. Dynamic-contrast enhanced MRI reflects tumour perfusion, whereas diffusion-weighted MRI measures water movement, which reflects on tumour cellular density and the integrity of the cellular membranes. MRI parameters, indicative of heterogeneous tumour perfusion and subtle tumour volume change early during chemo-radiotherapy, are independent and better predictors of tumour recurrence and death than clinical prognostic factors. Diffusionweighted imaging helps predict early response to chemo-radiotherapy in patients with advanced cervical cancer. Therefore, quantitative parameters generated from functional MRI techniques, such as perfusion and diffusion MRI, may serve as prognostic and predictive biomarkers in patients with cervical cancer.’
Future perspectives
One of the major future developments Dr Sala predicts is the use of hybrid imaging for cervical cancer. PET/MR combines local staging achieved through the superb soft tissue resolution of MRI with valuable metabolic information from PET. This brings together local staging and evaluation of distant metastases, which is important for therapy planning. Individualisation of patient treatment, assisted by quantitative hybrid imaging is clearly where the future is heading.
Profile:
Following medical studies at the University of Tirana Medical School in Tirana, Albania, Dr Evis Sala gained MPhil and PhD Degrees at the University of Cambridge, UK and took up a radiology residency at Cambridge University Hospitals. She also completed a Research Fellowship at Memorial Sloan-Kettering Cancer Centre, New York, USA, before returning to the University of Cambridge in 2005 as a University Lecturer/Honorary Consultant Radiologist. In July 2012, Dr Sala returned to Memorial Sloan-Kettering Cancer Center, to become Director of Gynaecologic Radiology. Her professional focus is on genitourinary cancer imaging; she has been awarded numerous awards and honours.
10.03.2013