Mental health and radiology
Eduardo de la Sota MD reports on the increasing use of radiology and neuro-imaging in psychiatry
The Uliazpi Foundation in Spain, which studies and cares for severely mentally retarded patients, carried out an interesting study to identify bone mineral density values in a group of its patients, compare these with the general population and investigate the possible influence on these values on certain clinical variables and therapeutic regimens.

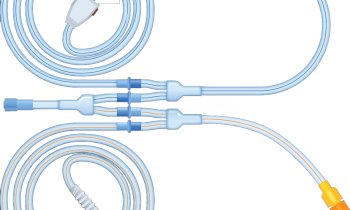
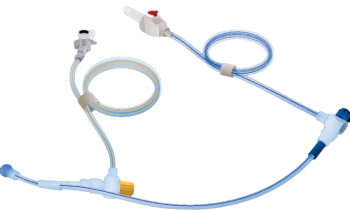
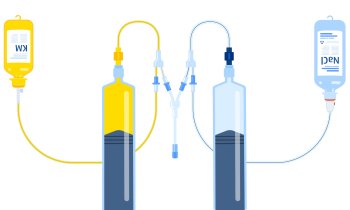
The bone mineral density value of 192 male/female patients was obtained via digital densitometry, using a compact desktop system with dual X-ray absorption measurement technology. The data obtained was contrasted with sex, age, degree of mobility and anti-epilepsy or sedative medication.
Mugica et al, found that the patients’ bone mineral density was significantly lower than that of the general population: 25% presented osteopenia and 22% osteoporosis. The latter is frequent among severely mentally retarded patients. The greatest risk is associated with insufficient mobility, Down’s syndrome and regular doses of Phenobarbital. The authors concluded that digital densitometry is a simple procedure that may be useful to identify the true
dimension of this problem
and the efficacy of the various preventive or curative procedures presented.
Neuro-imaging in Psychiatry (US)
The new ‘omics’ technologies (genomics, proteomics and metabolomics) heralded a new era of biomedical discovery that is affecting every field of medicine. With the rapid growth of the older population worldwide, there is great interest in applying these technologies not only to diagnose and prevent disease, but also to enhance brain longevity and mental wellness. Nearly two-thirds of the c. 30,000 genes in the human genome are related to brain function, and up to half of the variance in age-related changes in cognition, brain volume, and neuronal function appears to be genetically determined. Neuro-imaging is being employed to study the effects of genes and how neurogenetics may affect future radiology research and practice (Petrella et al, Department of Radiology, Duke University Medical Centre. Pub: 2008).
Mood disorders
Clinical research in mood disorders increasingly involves advanced neuro-imaging techniques. Advances in neuro-imaging technology have refined models of disease pathophysiology in mood disorders and the mechanistic basis of antidepressant action. Magnetic resonance (MR) approaches provide information on white and gray matter pathology (segmentation), cellular metabolism (MRS), oxygen consumption (BOLD), and neurocircuitry (DTI). Radionuclide-based neuro-imaging methodologies provide quantitative estimates of brain glucose metabolism, regional blood flow, and ligand-receptor/transporter binding. Clinical implications of neuro-imaging methodologies are widely recognised (Konarski et al. Canada).
Bipolar disorder
Strakowsky et al (2004) reviewed existing structural and functional neuro-imaging studies of patients with bipolar disorder and discussed how these investigations enhance our understanding of the neurophysiology of this illness. Findings from structural magnetic resonance imaging (MRI) studies suggest that some abnormalities, such as those in prefrontal cortical areas (SGPFC), striatum and amygdala exist early in the course of illness and, therefore, potentially, predate illness onset. In contrast, other abnormalities, such as those found in the cerebellar vermis, lateral ventricles and other prefrontal regions (e.g. left inferior), appear to develop with repeated affective episodes, and may represent the effects of illness progression and associated factors. Magnetic resonance spectroscopy investigations have revealed abnormalities of membrane and second messenger metabolism, as well as bioenergetics, in striatum and prefrontal cortex. Functional imaging studies report activation differences between bipolar and healthy controls in these same anterior limibic regions. Together, these studies support a model of bipolar disorder that involves dysfunction within subcortical (striatal–thalamic)–prefrontal networks and the associated limbic modulating regions (amygdala, midline cerebellum). These studies suggest that, in bipolar disorder, there may be diminished prefrontal modulation of subcortical and medial temporal structures within the anterior limbic network (e.g. amygdala, anterior striatum and thalamus) that results in dysregulation of mood. Future prospective and longitudinal studies focusing on these specific relationships are necessary to clarify the functional neuro-anatomy of bipolar disorder.
Brain scanning (Australia)
Nevertheless, CT has its limitations according to some researchers. Agzarian et al (2006) published research on the use of routine CT brain scanning of psychiatry patients in Australia. Their aim was to evaluate the usefulness of CT of the brain in patients presenting a psychiatric condition without focal neurological signs. The reports of 397 consecutive CT brain scans of patients at two acute tertiary hospital psychiatric services over a two-year period were assessed retrospectively. 377 (95%) of the CT scans showed no abnormality; specific abnormalities were described in 20 (5%). Three scans showed non-specific minor abnormalities, which, when followed up by MRI, showed no relevant abnormality. All the abnormalities shown on CT were considered clinically unrelated to the patient’s psychiatric condition. In conclusion, the pretest probability of finding a space-occupying lesion or other pertinent abnormality in the patients with psychiatric illnesses in this study appears not to be greater than that of the general population.
FMRI (Japan)
Functional magnetic resonance imaging (FMRI) has become the most widely used method for imaging normal brain function in a relatively short period of time. Its use in clinically related research has been much slower. However, FMRI is becoming a valuable tool in the study of many neurological and psychiatric disorders (Professor Matsuda. Japan).
01.03.2008