Live 3-D trans-oesophageal echocardiography
In 2007, Professor Andreas Franke, of Aachen University Medical Center, Germany, was the first cardiologist in Europe to perform minimally invasive cardiac catheterisation procedures under live 3-D ultrasound guidance.

This year he established this new modality in routine use in Siloah Hospital, at the Hanover Regional Medical Center.
Since the initial clinical applications, it became evident that the trans-oesophageal transducer yields crucial additional imaging data when closing an atrial septum defect, contributing significantly to a quicker, smoother procedure.
Cardiac catheter imaging and trans-oesophageal echocardiography (TEE) have been used since the mid-90s for defective septum closure. To image the heart without interference from ribs, fatty tissue, air in lungs, an ultrasound transducer is passed through the oesophagus. Previously, to assess the anatomical and spatial situation of the surgical site, 2 -D image sections had to be mentally assembled by the surgeon. The Philips development of a trans-oesophageal transducer delivering 3-D real-time images of the beating heart has improved the procedure immeasurably because data interpretation is quicker and easier, Prof. Franke confirms. ‘While conventional 2-D cross-sectional imaging focuses on a specific problem, the 3-D function delivers the entire spatial situation at a glance. This boosts the investigator’s confidence significantly during the procedure.’
The physician can assess the size of the finding and also clearly see the catheter as the atrial septal defect (ASD) is being closed. With this catheter a ‘double umbrella’ is positioned so that both its sides seal the septum defect. The catheter enters at the groin, proceeds into the right atrium and on through the septum defect in into the left atrium. He then expands the first umbrella, retracts the catheter, then the second umbrella is expanded in the right atrium, thus occluding the ASD.
The interaction of these imaging modalities is important. The examiner navigates the catheter under fluoroscopic guidance. However, this alone cannot delineate the atrial septal defect, so additional information is provided by 3-D ultrasound imaging. The rapidly beating heart is clearly seen and, as studies indicate, this procedure substantially reduces radiation exposure all round.
‘The development of live trans-oesophageal 3-D echocardiography may propel this modality to become the mainstay of many minimally invasive cardiac procedures,’ the professor predicts, adding: ‘In the future, it will become increasingly possible to avoid complex open heart surgery with its inherent long hospitalisation.’
The shift of live 3-D ultrasonography beyond its purely diagnostic function towards becoming a crucial element of an intervention is noticeable; it is a trend also evident in other imaging systems used in interventional radiology and surgery. The benefits are obvious in terms of patient comfort and shorter hospital stays.
Equipment summary
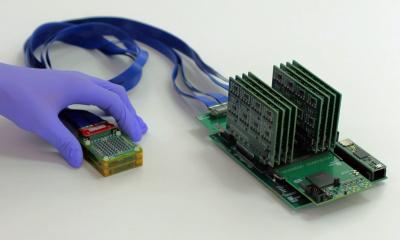
Live 3-D trans-oesophageal echocardiography (TEE) was developed by fusing and miniaturising two leading technologies in one probe: 3-D functionality of the xMATRIX and PureWave Crystal technologies. This allows visualisation of cardiac detail, pathologic changes and cardiac function in an absolutely novel fashion. The images generate additional information for diagnosis, treatment planning, monitoring and assessment during the intervention and the follow-up.
Live 3-D TEE imaging provides the interventional cardiologist with completely new perspectives on the heart: Mitral valve viewed from the left atrium and left chamber. Beating heart in real-time and in 3-D.
20.11.2008