
Image source: UMC Utrecht
News • Ultrafast power doppler imaging
Monitoring brain blood flow during surgery to prevent stroke
Thanks to a new technique, neurosurgeons at UMC Utrecht have been able to watch the blood flow in brain tissue live during surgery for the first time.
Together with researchers from Eindhoven University of Technology, they have developed a method that allows them to detect the risk of a stroke during surgery sooner – and potentially prevent it. The technique could also be useful for other types of operations, such as kidney transplants.
The researchers have published their findings in Nature Scientific Reports.
We saw effects that would otherwise only be visible afterward, when it is unfortunately too late, for example on an MRI scan. Now, we can already measure these effects during the surgery
Dara Niknejad
During surgeries on brain vessels, for example when treating an aneurysm or creating a bypass, there is a risk that the blood flow in brain tissue will temporarily stop. This can lead to a stroke. The risk of a stroke happening during aneurysm surgeries starts at around 8% and can rise to nearly 50% in complex cases. For brain tumors such as gliomas, the risk lies between 12.5% and 44%.
Until now, surgeons did not have a tool to directly observe a stroke during surgery. Thanks to a special type of ultrasound – Ultrafast Power Doppler Imaging (UPDI) – this has now changed. The technique visualizes the capillaries, measures the amount of blood in the brain tissue, and shows what happens during the procedure in real-time. This allows surgeons to immediately see whether the brain tissue receives enough blood during the temporary closure of a blood vessel. The technique is fast, safe, and easy to use during surgery.
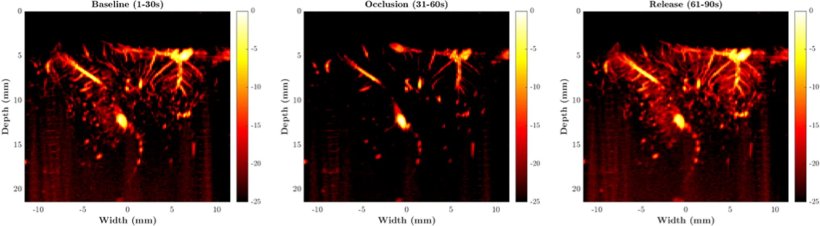
Image source: Niknejad HR, Huang Y, Auricchio AM et al., Scientific Reports 2025 (CC BY-NC-ND 4.0; cropped)
Researchers at UMC Utrecht tested the new technique on ten patients who underwent brain vessel surgery. During the procedure, they continuously measured blood flow changes in the brain tissue using the new ultrasound setup. In some cases, they could clearly see that the tissue received less blood, or temporarily more, just after removing a vascular clamp. “We saw effects that would otherwise only be visible afterward, when it is unfortunately too late, for example on an MRI scan. Now, we can already measure these effects during the surgery,” says neurosurgeon Dr. Dara Niknejad, who led the research.
The technique could also potentially be used in very different operations, says Dr. Niknejad. “It is useful for all surgeries where continuous blood flow to the tissue is critical. We haven’t tried it yet, but think about a kidney transplant, for example: the surgeon can immediately see whether the organ is fully perfused after transplantation. And even before the transplant, the organ can be assessed better with UPDI.”

Image source: UMC Utrecht
Prof. Dr. Massimo Mischi, chair of the Signal Processing Systems Group at Eindhoven University of Technology, adds: “The technology and expertise for using UPDI in this setting have been developed in our Biomedical Diagnostics lab. Dr. Yizhou Huang managed to use high-frequency, ultrafast ultrasound signals from multiple angles and process them to achieve high-resolution images of cerebral perfusion for the surgeons. Our accurate and high-resolution measurement of blood flow in the brain allows for early detection of reduced perfusion by quantitative analysis of UPDI, such that surgeons can take timely precautions during the operation and prevent severe complications, such as cerebral infarction.”
Every year, thousands of patients in the Netherlands undergo brain surgery for complications such as an aneurysm, a brain tumor, or a vascular malformation. Such surgeries may require a temporary closure of a brain blood vessel. This increases the risk of a stroke. With this new technique, researchers hope to better control that risk. “Our goal is to minimize complications. By looking at blood flow in real-time, we can intervene faster if something goes wrong,” says Dr. Niknejad.
The pilot is a first step. In follow-up research, the team aims to measure how well the technique can predict whether a patient will actually have a stroke. They also want to explore how to further integrate the technique into the operating room. Dara Niknejad: “Our ultimate goal is to make brain surgery safer, with fewer complications and better outcomes for patients.”
Source: UMC Utrecht
28.07.2025











