Article • Endoprosthetics
Joint efforts: New guidelines for arthroplasty
According to the Swedish Knee Arthroplasty Register, knee arthroplasty – with a revision rate of five percent after ten years – is one of the most successful surgical interventions of the post-World War II decades.
Report: Anja Behringer

The most frequent reasons for revision are loosening or infections, whereas patient dissatisfaction is often caused by mobility impairment and pain. Since many adverse events are associated with existing co-morbidities, the German Society for Endoprosthetics (AE) demands better patient information prior to surgery. Particularly, risks and benefits need to be more thoroughly discussed and unrealistic patient expectations regarding the implant need to be dampened.
Individual risks include infections, obesity, neurological disorders and other diseases. The psychological status of patients must also be considered, since depression, for example, can lead to frustration about slow healing or the situation in general. Moreover, cultural and social factors, such as a patient’s age and health status, can influence outcomes, says Professor Dr Karl-Dieter Heller, Medical Director of the Orthopaedic Clinic at Herzogin Elisabeth Hospital in Braunschweig, Germany, and Secretary General of AE. ‘The rule of thumb is: the better mobility and function are prior to surgery the better the outcomes.’
Too many surgeries?

Before arthroplasty is considered, all other therapy options should be exhausted: ‘Even when the X-ray shows severe arthritis, but the patient’s mobility is only slightly impaired and the patient is not in pain, we won’t perform surgery! About a third of patients referred to us for surgery are sent home, because we don’t consider an arthroplasty necessary. In real orthopaedic life, a fraction of patients with knee problems undergo arthroplasty – the first line treatment is conservation, i.e. joint-saving therapies,’ Heller points out. He recommends patience: ‘After surgery the healing process takes about half a year, after that the body should have become used to the implant.’ How long it will take to regain mobility and freedom from pain differs widely from patient to patient. Moreover, the healing process of hip and knee replacements are very different: a patient who received a new hip can move pretty well after two days, while a knee implant requires the patient to muster dedication and discipline throughout the physiotherapy phase.
In view of the fact that in time to come there won’t be a remedy for arthritis, endoprostheses play a major role. Nevertheless, for elderly patients being mobile is crucial for their overall health status. Recent studies indicate that arthritis-induced immobility is associated with a 40 percent increase in the risk of myocardial infarction compared to post-surgery activity. Lack of activity causes muscle atrophy – a serious problem according to Heller. To maintain mobility the pros and cons of conservative treatment, such as pain management and physiotherapy and, on the other hand, arthroplasty, need to be determined. The right decision for each individual can only be the result of an intensive communication process between physician and patient. After all, the knee is a highly complex anatomy and regaining its function is time-consuming.
New guidelines for the ‘forgotten knee’
These issues are addressed in guidelines on knee replacements, published by AE in late 2017. The recommendations on indication encompass primary and secondary criteria that aim to objectivise a patient’s subjective experience of pain and to include the patient in the decision-making process. Any discussion on volumes and quality needs to consider indications. In 2016 around 187,000 patients received a knee implant. Heller recommends selecting the orthopaedic surgeon carefully. In certified hospitals a surgeon has to perform a minimum of 50 implants per year. According to the guidelines, replacement surgery is indicated when ‘the knee is visibly damaged or the patient has been suffering from unbearable pain for three months’.
The arthroplasty patient also should be aware that s/he will not be able to follow a usual daily routine for up to three months and full rehabilitation may take up to two years, and also that s/he must be prepared to contribute to healing by complying with behavioural requirements. Since pain and impairment of mobility are subjective factors and culturally influenced and, since not every patient is fully aware of the risks involved in surgery, patients evaluate the outcomes very differently.

One of the, albeit rare, post-surgery adverse events is implant loosening. Infections and instability and pain behind the patella, or frontal knee pain, occur more frequently and might indicate an incorrectly positioned implant or incorrect ligament alignment during surgery. In any case, the causes must be ascertained. Increased risk of implant failure is also associated with obesity and comorbidities such as gout, diabetes, rheumatism and neurological disorders such as Parkinson’s disease. Moreover chronic infections, e.g. of the bladder or teeth need to be cured before surgery, because bacteria can spread and infect the implant.
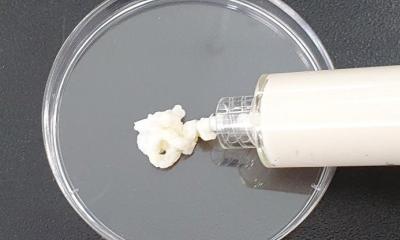
Today, infections are considered the major risk in arthroplasty. If a patient turns out to carry an infection prior to surgery, the intervention is postponed. ‘Infections are a serious adverse event in only about one percent of initial implantations. However, in revision, and above all tumour arthroplasty, the infection rate is significantly higher,’ Heller points out. Fortunately, silver-coated replacement joints can reduce the infection rate.
Profile:
Professor Karl-Dieter Heller MD studied medicine in Aachen, Germany, and London, UK, in 1983. Following completion of his habilitation, in 1997 he received the venia legendi in orthopaedics from Rheinisch-Westfälische Technische Hochschule Aachen. He was appointed medical director of the Orthopaedic Clinic in Braunschweig in 2000 and has been secretary general of the German Society for Endoprosthetics (AE) since 2015. In 2016 Heller became a founding member and vice president of the German Hip Society (DHG). His awards and honours are numerous and he is active in several surgery and orthopaedic as well as professional organisations.
06.02.2019